Received: Mon 16, Oct 2023
Accepted: Wed 15, Nov 2023
Abstract
Objectives: This study aimed to assess the influence of abdominal computerized tomography (CT) scans on the management of children presenting with acute abdominal conditions, considering concerns regarding radiation exposure. Methods: A retrospective review was conducted of all acute pediatric patients who underwent abdominal CT in a tertiary hospital, during 2018-2019. Results: Over the 2-year period, 976 pediatric patients were admitted due to acute abdominal conditions. Of 197 (20.2%) patients who underwent abdominal CT scans, management plan was modified based on CT results in 67.5%. In non-trauma cases, the impact on the management plan was even more pronounced, affecting 91.2% of patients, and led to invasive procedures (one third), non-invasive actions (one third), or discharge (one third). Multivariate analysis demonstrated a significantly higher odds ratios (OR) for impact on management in non-trauma patients (OR=24) as compared to trauma patients, especially younger (OR=1.58 annually) and male (OR=10.42) patients, and when performed early (OR=2.44, for each day earlier). Trauma patients with a lower body mass index (BMI) (OR=1.02 per percentile decrease) demonstrated a significantly larger impact. Conclusion: These results support a more liberal use of early CT scans in non-traumatic acute pediatric abdominal conditions, especially in younger male patients, with more careful consideration in trauma patients, particularly those with high BMIs.
Keywords
Abdominal CT, management, pediatric, acute abdominal conditions
1. Introduction
In recent years, there has been a growing body of literature on the potential risk of malignant neoplasms resulting from exposure to computerized tomography (CT) radiation [1-3]. Some authors, however, argue that data on radiation damage is not applicable to CT scans, and that avoiding CT scans may result in missed diagnoses and inappropriate treatment [4, 5]. While guidelines have been developed to reduce the use of abdominal CT scans in trauma patients [6-9], little is known about the impact of CT scans on management decisions for acute non-trauma pediatric abdominal conditions. Previous studies have explored the use of CT scans for diagnosing appendicitis in children [10, 11], but the broader impact of abdominal CT scans on the management of non-trauma pediatric patients remains unclear.
This study aims to evaluate the role of abdominal CT scans in the management of acute pediatric abdominal conditions, both in trauma and non-trauma settings, and to identify patient factors associated with a bigger impact on management.
2. Materials and Methods
Data was retrospectively retrieved, during 2018-2019, for all patients admitted to the pediatric surgical service from the emergency department in a tertiary medical center, who underwent an abdominal CT scan during admission. Only patients admitted due to acute abdominal/gastrointestinal conditions or acute abdominal trauma were included. The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Shamir Medical Center (protocol code 0221-18-ASF October 3, 2018). Patient consent was waived due to the retrospective nature of the study without a therapeutic intervention.
Data retrieved included demographic, clinical, imaging, laboratory, and management parameters, including patient age, sex, working diagnosis (prior to performing CT), body mass index (BMI) percentile, timing of CT scan relative to admission, CT diagnosis, if x-rays and ultrasound (US) were done, impact of CT diagnosis on treatment, and length of stay (LOS). White blood count (WBC) and C-reactive protein (CRP) were analyzed for non-trauma patients, and aspartate aminotransferase (AST), alanine aminotransferase (ALT), lipase, and amylase were analyzed for trauma patients.
Working diagnoses were classified as trauma versus non-trauma. Non-trauma diagnoses were further classified as: appendicitis, inflammatory bowel disease, intra-abdominal collection, abdominal mass, gynecological, bowel obstruction, and unspecified abdominal pain.
CT diagnoses were grouped into four groups: normal study, positive trauma associated injury, appendicitis (including periappendicular abscess), and other. "Other" included enteritis/colitis, any intra-abdominal collection (including post-appendectomy but excluding periappendicular abscess), gynecological, abdominal mass, mesenteric lymphadenitis, incidental findings, and bowel obstruction.
Possible impact on management was categorized into one of four options: no change; discharge on the day of CT scan; pursuing an invasive treatment (surgery, endoscopic retrograde cholangiopancreatography (ERCP), percutaneous drainage) following the results of the CT scan; and non-invasive actions taken following the results of the CT scan (transfer to another service, starting a new pharmacological treatment, or pursuing additional diagnostic evaluation). For statistical analysis purposes, the different categories were grouped as no change in management versus revised management (all other options combined).
Univariate and multivariate analyses were conducted to evaluate whether specific patient factors were associated with revision of management following the results of CT scans. We analyzed the entire population as one group, and trauma and non-trauma patients separately.
2.1. Statistical Analysis
Categorical variables were reported as frequency and percentage. Normally distributed continuous variables were evaluated using histograms and reported as mean and standard deviation, or if not normally distributed as median and interquartile range. Chi-square test or Fisher exact test were used to compare categorical variables. Ordinal and continuous variables were compared using Mann-Whitney test or independent samples t-test. Multivariable analysis was performed using logistic regression. All statistical tests were two sided. P<0.05 was considered statistically significant. SPSS software, version 24 (IBM SPSS statistics, IBM Corp, Armonk, NY, USA) was used to perform the statistical analysis.
3. Results
During 2018-2019, a total of 976 patients were admitted to the pediatric surgical service due to acute abdominal conditions. Of them, 197 (20.2%) patients who underwent an abdominal CT scan included 77/200 (38%) trauma patients and 125/776 (16%) non-trauma patients. For the entire group, median age was 13.4 (9.8-16.3) years, with 106 (54%) males and 91 (46%) females. Median BMI percentile was 71 (36.2-91.7). In 88 (45%) patients a CT scan was performed while in the emergency department (ED), while in 109 (55%) patients it was performed later, when the patients were already in the surgical ward. Median time from admission to obtaining a CT scan was 0 (0-1) days. Median LOS was 2 (1-4) days. In 127 (64%) patients one or more US scans were carried out prior to performing a CT scan; however, they were either non diagnostic or non-conclusive. In 24 (10%) patients an abdominal X-ray prior to performing a CT scan was done; however, it was either non diagnostic or non-conclusive. Of note, liver and pancreatic enzymes (AST, ALT, amylase, and lipase) were examined in only 43 (60%), 43 (60%), 40 (55%), and 34 (47%) of the 72 trauma patients, respectively. WBC and CRP, however, were evaluated in 123 (98%) and 124 (99%) of non-trauma patients. Figure 1 presents the distribution of cases according to the different classes of working diagnoses and CT diagnoses within the entire study group.
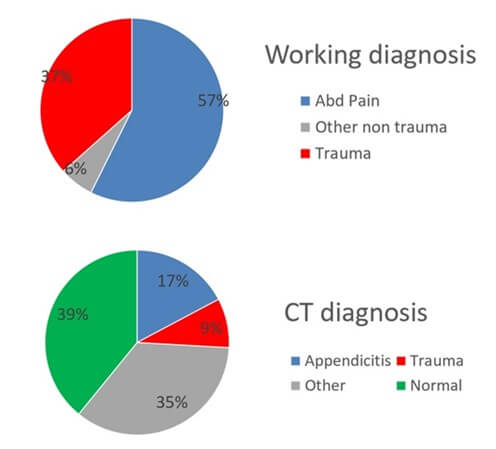
Table 1 presents the distribution of cases in which management was revised versus cases with no change in management following CT for the entire study population, and among trauma versus non-trauma patients. Figure 2 presents revisions of patient management plans following CT within trauma and non-trauma groups separately.
TABLE 1: Management
following CT scan in trauma and non- trauma patients.
|
|
Total |
Trauma |
Non-Trauma |
P* |
|||
|
|
Number of
cases |
Percentage of cases |
Number of
cases |
Percentage of cases |
Number of cases |
Percentage of cases |
|
|
No change in management |
64 |
32.5% |
53 |
74% |
11 |
8.8% |
<0.001 |
|
Revision in management |
133
|
67.5% |
19 |
26% |
114 |
91.2% |
<0.001† |
|
Discharge |
43 |
21.8% |
5 |
6.9% |
38 |
30.4% |
|
|
Invasive |
42 |
21.3% |
4 |
5.5% |
38 |
30.4% |
|
|
Non-invasive |
48 |
24.4% |
10 |
13.9% |
38 |
30.4% |
|
|
Total |
197 |
100% |
72 |
100% |
125 |
100% |
|
*When
comparing Trauma to Non-Trauma. †also significant when comparing each category
of management change between trauma and non-trauma patients.
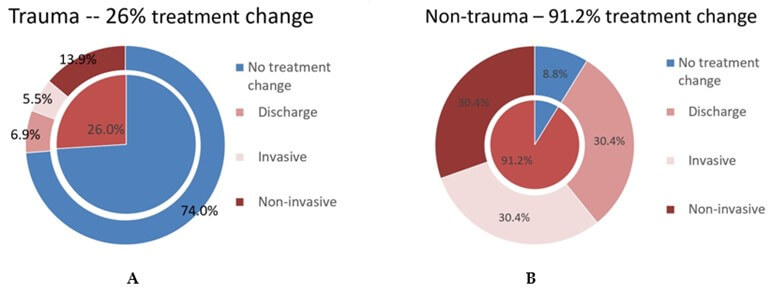
It can be appreciated that, following the results of abdominal CT, management was revised in 91% of all non-trauma patients. In one third, an invasive procedure was pursued, in one third a non-invasive action was taken, and in one third a decision to discharge the patient home on the same day was made. Of note, management was revised in only 26% of trauma patients, with only 5.5% percent of them undergoing an invasive procedure following the results of the CT scan.
3.1. Univariate Analysis for Possible Associations with Revision of Management Following CT
Table 2 presents the results of univariate analyses conducted to examine associations between patient factors and possible impacts on management for the entire group, and within the trauma versus non-trauma groups.
TABLE 2: Univariable analysis for patient
factors associated with revision of management following CT scan.
* Significant for comparing all subcategories except
for trauma.
ALT:
Lipase, and Amylase were Analyzed; AST: Alanine Aminotransferase; BMI: Body
Mass Index; CRP: C-Reactive Protein; CT: Computerized Tomography; LFT: liver
function tests; LOS: Length Of Stay; WBC: White Blood Count.
Within the entire group, revision of management was significantly associated with older age, CT diagnosis of appendicitis, delayed versus early CT, and male sex. Amongst patients admitted due to trauma, revision of management was significantly associated with delayed versus early CT, lower BMI percentile, and longer LOS. Also, management was revised in 38% of trauma patients in whom liver function tests (LFT) were not checked, and in only 18% of patients in whom LFTs were checked, with a trend towards significance (P= 0.068). Among non-trauma patients, revision of management was significantly associated with an earlier versus a delayed CT, increased WBC, and increased CRP.
3.2. Multivariate Analysis for Patient Factors Associated with Revision of Management Following CT
Table 3 presents the results of the multivariate analysis. For the entire group, the odds ratio (OR) for revision of management significantly increased with non-trauma admission diagnosis versus trauma (OR=24), and for patients with a lower BMI percentile (OR=1.02 per percentile decrease). Among trauma patients, the OR for revision in management significantly increased only for patients with a lower BMI percentile (OR=1.02 per percentile decrease). Amongst the non-trauma patients, the OR for revision in management increased with younger age (OR=1.58 per year younger), in male patients (OR=10.42), and when the CT scan was performed earlier (OR=2.44 decrease for each day earlier).
TABLE 3: Multivariate analysis for patient
factors associated with revision in management following CT scan.
|
|
Total |
Trauma |
Non-Trauma |
|||||||
|
|
OR |
Interval |
P |
OR |
Interval |
P |
OR |
Interval |
P |
|
|
Age (per year younger) |
1.05 |
0.91-1.19 |
0.41 |
0.95 |
0.13-2.77 |
0.57 |
1.58 |
1.06-2.38 |
0.023 |
|
|
Sex (male/female) |
1.72 |
0.59-5 |
0.32 |
0.59 |
0.81-1.12 |
0.51 |
10.4 |
1.05-100 |
0.045 |
|
|
BMI percentile (per percentile decrease) |
1.02 |
1.02-1.03 |
0.021 |
1.02 |
1.01-1.04 |
0.041 |
1 |
0.97-1.03 |
0.98 |
|
|
admission diagnosis (non-trauma/ trauma) |
24.39 |
4.54-125 |
<0.001 |
|
|
|
|
|
|
|
|
CT day from admission (for each day earlier) |
0.89 |
0.89-1.85 |
0.16 |
0.37 |
0.07-2.04 |
0.25 |
2.44 |
1.2-5 |
0.013 |
|
BMI:
Body Mass Index; CT: Computerized Tomography.
4. Discussion
We have demonstrated that abdominal CT scans have a significant impact on the management of children with acute abdominal conditions, which led to a subsequent revision of management in 67.5% of patients. This benefit was more pronounced in non-trauma patients, in whom management was revised in 91.2% of cases. Our key findings reveal that patients with a lower BMI benefited more from undergoing abdominal CT in trauma cases, while younger male patients who underwent an early CT saw the most significant benefit among non-trauma patients.
Our findings reinforce robust data from previous studies that evaluated the contribution of abdominal CT scans for diagnosis and treatment in pediatric trauma patients [8, 11, 12]. These studies challenged the criteria for performing abdominal CT scans for pediatric trauma and found that the use of CT for assessment of injuries could be reduced without compromising patient safety [8-11, 13]. It is important to note that although many of these studies relied on LFTs (and pancreatic enzymes) for imaging criteria, with the classic ALT/AST cutoff levels of 200/125 U/l, in our study liver and pancreatic enzymes were checked in only 47% - 60% of trauma patients. In addition, a nearly significant finding in our study was that management was revised following CT in 38% of trauma patients in whom LFTs were not checked, and in only 18% of patients in whom LFTs were checked. Perhaps the discrepancy between these two groups may be explained by CT scans that were used for "screening" rather than appropriate blood analysis, and therefore, fewer noncontributory CT scans were obtained when LFTs were checked. A possible explanation for the relatively low rate of checking LFTs in our study population might be that in our institution pediatric trauma patients are sometimes evaluated by adult trauma surgeons. Many previous studies have demonstrated worse outcomes and more unnecessary CT scans performed in adult trauma centers as compared to pediatric trauma centers [14, 15]. Adult trauma surgeons might feel more uncomfortable evaluating children, and this might result in more unnecessary CTs being performed. Adult surgeons might also be unfamiliar with the recommendation for screening blood work in pediatric trauma patients.
We show that abdominal CT has a very high impact on management of non-trauma patients. While some studies have demonstrated a high diagnostic yield of CT scans in pediatric appendicitis [16, 17], we did not find any articles describing the yield of abdominal CT in non-trauma patients in general. Only 17.3% of CT diagnoses in our group were appendicitis.
Our multivariate analysis demonstrated that the impact on treatment of non-trauma patients was less when a CT scan was delayed or used in older or female patients. In the latter post-pubertal female population, confounding diagnoses such as gynecological and functional disorders are more prevalent [18], for which there is no specific treatment, and in whom abdominal pain can persist, delaying discharge even with a negative CT scan.
CT has not been used as the primary diagnostic tool for evaluating non-trauma pediatric patients in our institution. Laboratory tests, US, and observation are the common tools used for primary evaluation. Our univariate analysis demonstrated that when blood inflammatory markers (WBC and CRP) were elevated, the impact of CT on management was increased. This finding may support avoiding CT if inflammatory blood markers are not elevated.
In the multivariate analysis for trauma patients, the only variable associated with high impact on management was BMI percentile, with a lower BMI associated with a larger impact. Roy et al. [19] found that obese children and adolescents undergo more abdominal CT scans than non-obese patients, possibly due to difficulties with physical examination and ultrasound reading. This also might be the explanation for the lower impact on management in trauma patients with a higher BMI, as patients with a higher BMI undergo more unnecessary CT scans.
Our univariate analysis for trauma patients revealed that when CT was delayed, its yield increased. Traditionally, abdominal CT in trauma patients is performed immediately upon patient arrival. Our findings might support clinical observation in trauma patients who are not highly suspected to have suffered an intraabdominal injury, as superior to early CT scan.
Lastly, current CT scanners offer equivalent diagnostic accuracy to older scanners, but with significantly reduced radiation levels [20-22]. As a result, clinicians are now able to use CT scans more liberally. However, it is important that radiation risks, as demonstrated by many studies including recent ones (1-3), should still concern the clinician. Therefore, it is essential for clinicians to carefully consider the benefits of CT scans on a case-by-case basis while weighing the associated risks of radiation.
Selecting the patients who will benefit from an abdominal CT scan can increase diagnostic accuracy when CT is indicated, and decrease risks, time and discomfort associated with contrast administration and patient preparation when CT is not likely to be beneficial. Thus, both short- and long-term patient outcomes can improve, as well as patient and family quality of life.
5. Conclusion
Abdominal CT significantly impacts the management of acute non-trauma pediatric patients. Impact decreases if the scan is delayed, done in older females, or when performed in trauma patients, particularly those with a higher BMI, emphasizing caution in CT usage in these patients. These conclusions might inform clinical guidelines on the use of abdominal CT in acute pediatric patients, as well as guide further research on this topic, particularly randomized controlled trials.
Limitations
The study was conducted at a single center, which may limit its generalizability due to potential local population and practice confounders. Moreover, our study was retrospective and did not include a control group in which CT was not performed, nor was it controlled for inclusion/exclusion criteria for performing a CT scan. In addition, as a non-randomized trial a selection bias is inherent. This selection bias might affect the results and preclude conclusions on the possible role of CT in cases that were not selected to undergo CT.
Author Contributions
Conceptualization, O.Z, R.B and A.I.; methodology, O.Z, A.I. G.B, V.K, R.B and N.A.; software, O.Z, R.A, A.I. G.B. V.K. and N.A; validation, O.Z and A.I.; formal analysis, R.A, O.Z and A.I.; investigation, O.Z and A.I.; data curation, O.Z, A.I, G.B, V.K and N.A.; writing-original draft preparation, O.Z.; writing-review and editing, R.A, R.B, O.Z, A.I and N.A.; supervision, O.Z.; project administration, O.Z and R.B;. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
None.
Funding
None.
Acknowledgments
The authors would like to thank Dr. Tomer Ziv-Baran for his assistance with study design and with statistical analysis.
REFERENCES
[1] David J
Brenner “Estimating cancer risks from pediatric CT: Going from the qualitative
to the quantitative.” Pediatr Radiol, vol. 32, no. 4, pp. 228-231, 2002.
View at: Publisher
Site | PubMed
[2] Diana L
Miglioretti, Eric Johnson, Andrew Williams, et al. “The use of computed
tomography in pediatrics and the associated radiation exposure and estimated
cancer risk.” JAMA Pediatr, vol. 167, no. 8, pp. 700-707, 2013. View at:
Publisher
Site | PubMed
[3] Kyung Hee
Lee, Seungjae Lee, Ji Hoon Park, et al. “Risk of Hematologic Malignant
Neoplasms from Abdominopelvic Computed Tomographic Radiation in Patients Who
Underwent Appendectomy.” JAMA Surg, vol. 156, no. 4, pp. 343-351, 2021.
View at: Publisher
Site | PubMed
[4] Savvas
Andronikou “Letting go of what we believe about radiation and the risk of
cancer in children.” Pediatr Radiol, vol. 47, no. 1, pp. 113-115, 2017.
View at: Publisher
Site | PubMed
[5] Mervyn D
Cohen “Reply to Dr. Andronikou: Disavowing the ALARA concept in pediatric
imaging.” Pediatr Radiol, vol. 47, no. 1, pp. 116-117, 2017. View at: Publisher
Site | PubMed
[6] Mervyn D
Cohen “Point: Should the ALARA Concept and Image Gently Campaign Be
Terminated?” J Am Coll Radiol, vol. 13, no. 10, pp. 1195-1198, 2016.
View at: Publisher
Site | PubMed
[7] R Paul
Guillerman “From ‘Image Gently’ to image intelligently: a personalized
perspective on diagnostic radiation risk.” Pediatr Radiol, vol. 44 Suppl
3, pp. S444-S449, 2014. View at: Publisher Site | PubMed
[8] Michaela
Gaffley, Lucas P Neff, Leah M Sieren, et al. “Evaluation of an evidence-based
guideline to reduce CT use in the assessment of blunt pediatric abdominal
trauma.” J Pediatr Surg, vol. 56, no. 2, pp. 297-301, 2021. View at: Publisher Site | PubMed
[9] Jessica A
Zagory, Avafia Dossa, Jamie Golden, et al. “Re-evaluation of liver transaminase
cutoff for CT after pediatric blunt abdominal trauma.” Pediatr Surg Int,
vol. 33, no. 3, pp. 311-316, 2017. View at: Publisher Site | PubMed
[10] Shweta
Bharadwaj, Joshua Rocker “Minor head injury: Limiting patient exposure to
ionizing radiation, risk stratification, and concussion management.” Curr
Opin Pediatr, vol. 28, no. 1, pp. 121-131, 2016. View at: Publisher
Site | PubMed
[11] Christine M
Leeper, Isam Nasr, Abigail Koff, et al. “Implementation of clinical
effectiveness guidelines for solid organ injury after trauma: 10-year
experience at a level 1 pediatric trauma center.” J Pediatr Surg, vol.
53, no. 4, pp. 775-779, 2018. View at: Publisher Site | PubMed
[12] Anurag
Jindal, George C Velmahos, Roya Rofougaran “Computed tomography for evaluation
of mild to moderate pediatric trauma: Are we overusing it?” World J Surg,
vol. 26, no. 1, pp. 13-16, 2002. View at: Publisher Site | PubMed
[13] Eric R
Scaife, Michael D Rollins “Managing radiation risk in the evaluation of the
pediatric trauma patient.” Semin Pediatr Surg, vol. 19, no. 4, pp.
252-256, 2010. View at: Publisher
Site | PubMed
[14] Ashley E
Walther, Richard A Falcone, Timothy A Pritts, et al. “Pediatric and adult trauma
centers differ in evaluation, treatment, and outcomes for severely injured
adolescents.” J Pediatr Surg, vol. 51, no. 8, pp. 1346-1350, 2016. View
at: Publisher
Site | PubMed
[15] Ashley E
Walther, Timothy A Pritts, Richard A Falcone, et al. “Teen trauma without the
drama : Outcomes of
adolescents treated at Ohio adult versus pediatric trauma centers.” J Trauma
Acute Care Surg, 77, no. 1, pp. 109-116, 2014. View at: Publisher
Site | PubMed
[16] Antonia E
Stephen, Dorry L Segev, Daniel P Ryan, et al. “The diagnosis of acute
appendicitis in a pediatric population: To CT or not to CT.” J Pediatr Surg,
vol. 38, no. 3, pp. 367-371, 2003. View at: Publisher Site | PubMed
[17] C J Sivit, K
E Applegate, A Stallion, et al. “Imaging evaluation of suspected appendicitis
in a pediatric population: Effectiveness of sonography versus CT.” Am J
Roentgenol, vol. 175, no. 4, pp. 977-980, 2000. View at: Publisher
Site | PubMed
[18] S Palomba, A
Di Cello, E Riccio, et al. “Ovarian function and gastrointestinal motor
activity.” Minerva Endocrinol, vol. 36, no. 4, pp. 295-310, 2011. View
at: PubMed
[19] Haven Roy,
Brent Burbridge “To CT or not to CT? The influence of computed tomography on
the diagnosis of appendicitis in obese pediatric patients.” Can J Surg,
vol. 58, no. 3, pp. 181-187, 2015. View at: Publisher Site | PubMed
[20] Yasunori
Nagayama, Seitaro Oda, Takeshi Nakaura, et al. “Radiation dose reduction at
pediatric CT: Use of low tube voltage and iterative reconstruction.” Radiographics,
vol. 38, no. 5, pp. 1421-1440, 2018. View at: Publisher Site | PubMed
[21] Thomas R
Goodman, Adel Mustafa, Erin Rowe “Pediatric CT radiation exposure: where we
were, and where we are now.” Pediatr Radiol, vol. 49, no. 4, pp.
469-478, 2019. View at: Publisher
Site | PubMed
[22] Abigail
Bryce-Atkinson, Rianne De Jong, Tom Marchant, et al. “Low dose cone beam CT for
paediatric image-guided radiotherapy: Image quality and practical
recommendations.” Radiother Oncol, vol. 163, pp. 68-75, 2021. View at: Publisher
Site | PubMed
[23] Takuya Nishizawa, Shigenobu Maeda, Ran D Goldman, et al. “Predicting need for additional CT scan in children with a non-diagnostic ultrasound for appendicitis in the emergency department.” Am J Emerg Med, vol. 36, no. 1, pp. 49-55, 2018. View at: Publisher Site | PubMed
[24] Baruch Klin, Leonid Zlotcavitch, Oleg Lysyy, et al. “Complicated appendicitis wrongly diagnosed as nonspecific diarrhea: ways to decrease this continuous threat.” Minerva Pediatr. (Torino), vol. 75, no. 1, pp. 14-20, 2023. View at: Publisher Site | PubMed
