Received: Fri 24, Nov 2023
Accepted: Tue 26, Dec 2023
Abstract
Radicular cysts are one of the most commonly occurring cysts in the jaw, with an occurrence rate of 54.6% amongst odontogenic cysts. After removal of the cyst, there tends to be a large bony defect, resulting in a buccal concavity, especially when the buccal cortex has been eroded by the cyst. This compromises aesthetic outcomes where prosthodontics rehabilitation is considered in the future. Here we describe two cases of reconstruction of cystic defects with resorbable membranes, supported by a stable framework of “shoelace” sutures, with the objective of improving hard and soft tissue healing with minimal buccal collapse. This technique is useful in supporting resorbable membranes placed above the defect and can potentially reduce the extent of hard and soft tissue deficiency.
Keywords
Radicular cyst, odontogenic cyst, defect, aesthetic, sutures
1. Introduction
Radicular cysts are one of the most commonly occurring cysts in the jaw, with an occurrence rate of 54.6% amongst odontogenic cysts [1]. They tend to occur more commonly in the maxillary anterior region and have a higher predilection for males. The frequency of radicular cysts has been shown to peak between the third and fifth decades. Although rare, they can also occur amongst children in deciduous teeth [2].
Radicular cysts arise due to long-standing inflammatory processes in the bone of the root apex, with proliferation of epithelial rests of malassez [3]. They are commonly treated with conventional root canal therapy of the offending tooth, followed by surgical enucleation of the cyst and simultaneous apicectomy. For larger cysts, some authors had suggested initial marsupialization, followed by an eventual enucleation after reduction of size. de Castro et al. [4] found that cysts treated with marsupialization followed by enucleation displayed superiority of success compared to initial enucleation. Minor total recurrence rate was lower (17.8%) for cysts treated with marsupialization followed by enucleation, in contrast with enucleation alone (20.8%).
The resulting bone defect can be reconstructed with bone grafts, resorbable membranes, or left alone to heal spontaneously. In current literature, there is no consensus on the more superior option [5]. However, with spontaneous healing, there will be extensive bone and soft tissue remodeling, creating a buccal concavity, especially when the buccal cortex has been eroded by the cyst. This unfortunately compromises aesthetic outcomes where prosthodontic rehabilitation is considered in the future. Furthermore, extensive alveolar bone grafting may be needed to augment horizontal bone deficiency, should a dental implant be indicated.
This case series describes the reconstruction of cystic defects with resorbable membranes, supported by stable frameworks of “shoelace” sutures, with the objective of improving hard and soft tissue healing with minimal buccal collapse.
2. Case Series
2.1. Case 1
An 11 year-old boy was referred to National Dental Centre Singapore (NDCS) with an anterior maxillary labial swelling. He had history of trauma to the anterior maxilla in 2018 during which the upper right central incisor (#11) sustained an uncomplicated enamel-dentine fracture. The tooth was diagnosed as necrotic and endodontic treatment was initiated in 2018 but remained uncompleted.
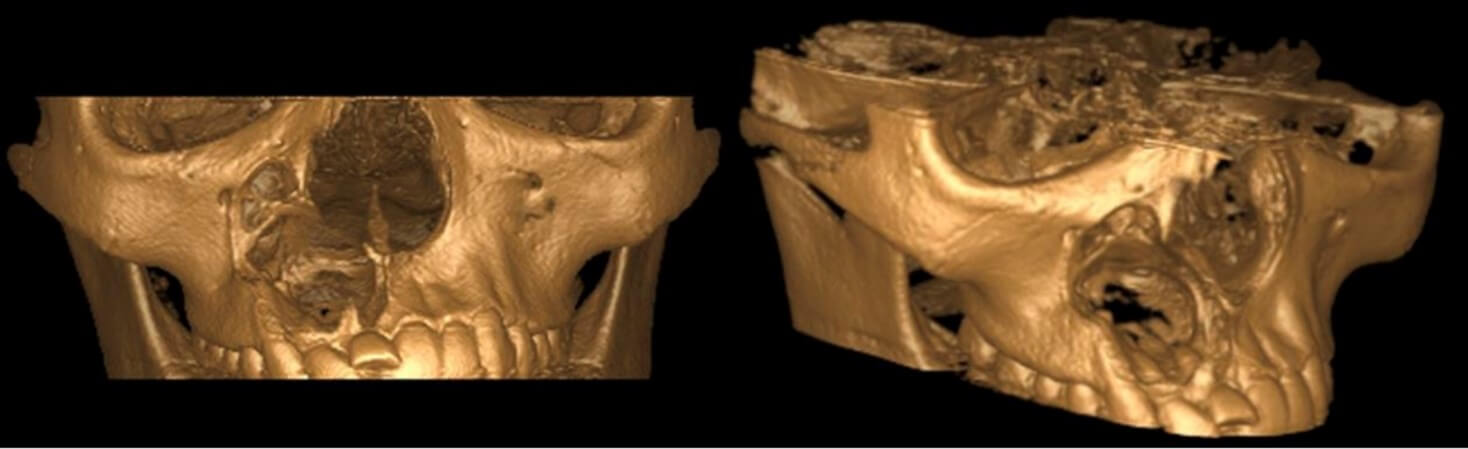
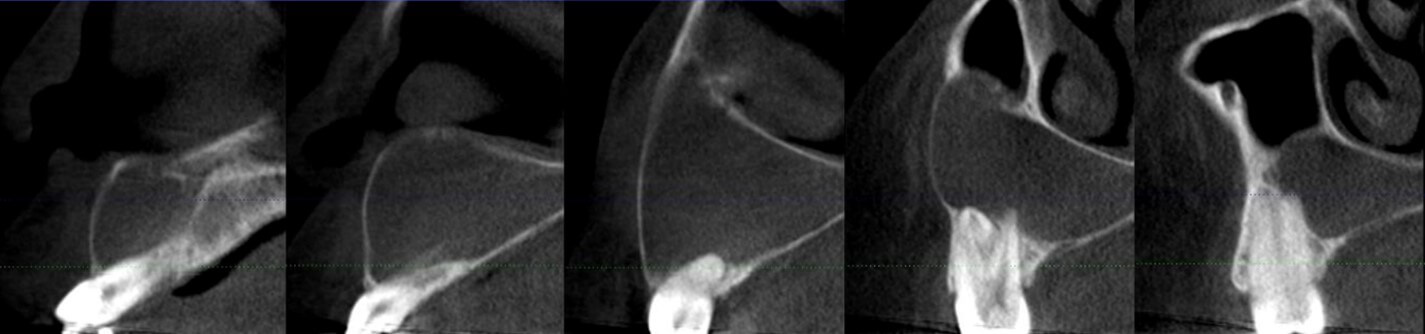
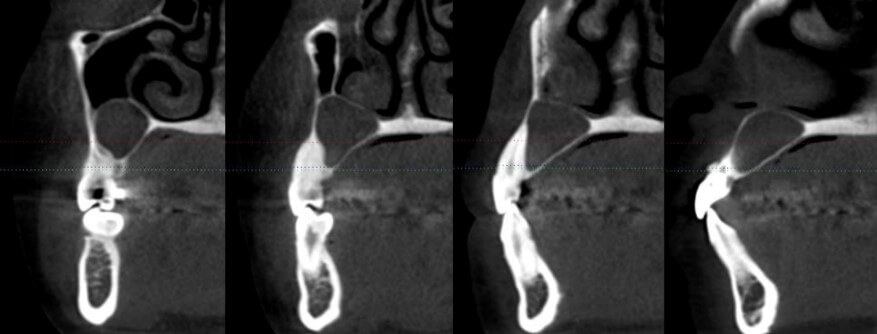
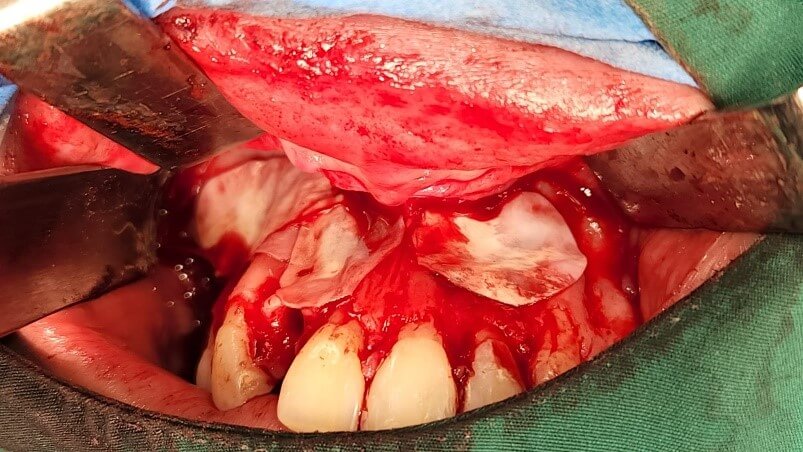
Cone-beam computed tomography (CBCT) and periapical radiograph revealed a large radiolucency extending from the apex of #11 to the upper right canine (#13), measuring 25 mm by 27 mm. There was erosion of labial bone and expansion of the lesion into the nasal floor and maxillary sinus (Figures 1 & 2). Histopathological findings from an initial incisional biopsy were consistent with a radicular cyst. Conventional root canal treatment was completed for #11 and the patient was planned for surgical enucleation of the cyst and simultaneous apicoectomy. During the surgery, a buccal mucoperiosteal flap was raised and the cyst was fully enucleated with cystic lining intact (Figure 3). Peripheral bone was minimally removed with a bur to gain access for apicoectomy.
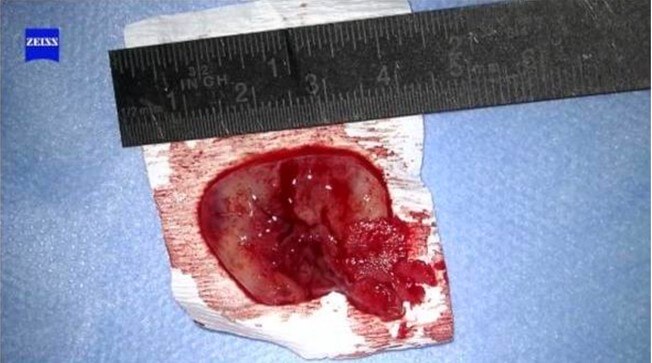
The eventual cystic defect approximated 3 cm by 3 cm. A small round bur was used to create holes along the bony border of the defect. Three holes were placed on the left and right borders each, with all holes positioned approximately 3 mm equidistant from one another. 5/0 vicryl sutures were threaded diagonally across these holes, mimicking a shoe-lace pattern (Figure 4).
A bovine pericardium acellular collagen matrix Tutopatch membrane (RTI Biologics, TUTOGEN Medical GmbH, Germany) was cut to the approximate size of the defect, covering 2mm of the bony margins. The membrane was propped up above the “shoelace” sutures (Figure 5). The buccal flap was then repositioned and sutured with 5/O vicryl sutures (Figure 6). Good healing with maintenance of labial bone projection was observed at 2-week post-operative review (Figure 7).




2.2. Case 2
A 29 year-old female was referred to NDCS for management of cystic lesions associated with the upper right and left central and lateral incisors (#11, #21, #12, #22). #11 and #12 were previously root canal treated and restored with veneers more than 10 years ago. #22 was necrotic but did not have prior root canal treatment.
CBCT and periapical radiographs revealed a well-defined radiolucent lesion extending from the apices of #11 to the upper right second premolar (#15), and a separate well-defined radiolucency extending from #21 to the upper left canine (#23) (Figures 8-10). External root resorption was also observed on #12.
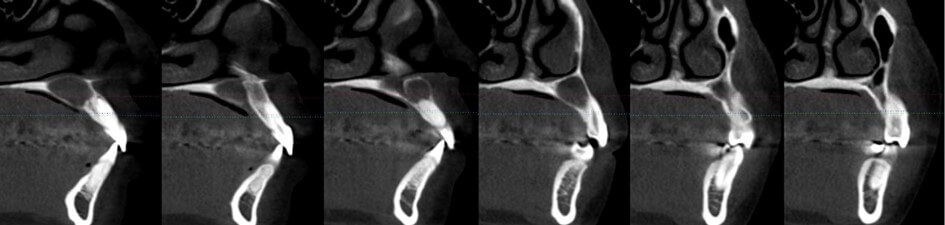
During the incisional biopsy, buccal cortex perforation was noted apical to the upper right canine and first premolar (#13, #14). There was also disruption of the right maxillary sinus floor, with the sinus membrane in direct contact with the cystic lining. The cystic lesion was associated with the previously endodontically treated #12 and #11. Results of the incisional biopsy were consistent with a radicular cyst. Conventional root canal treatment was completed for #22 and patient was planned for surgical enucleation of the cystic lesion and simultaneous apicoectomy of #22.
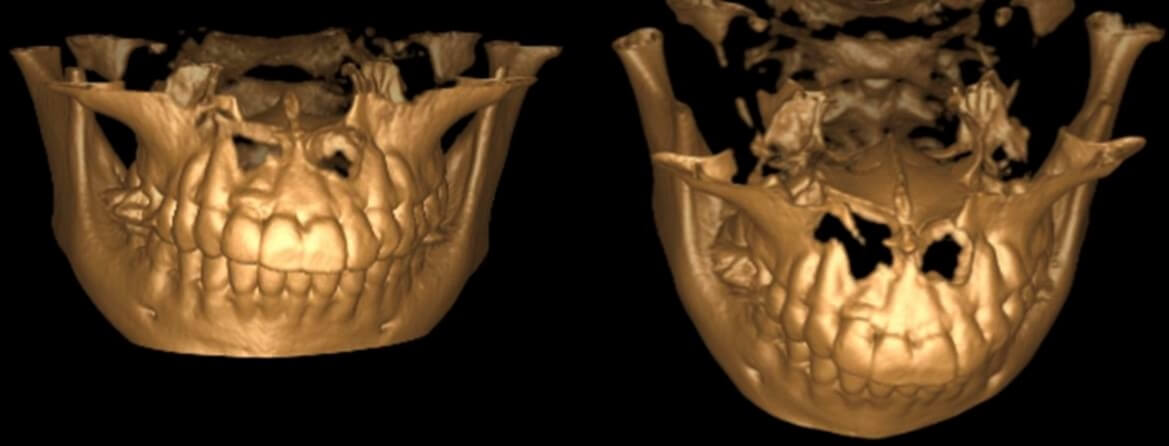
During the surgery, a buccal mucoperiosteal flap was raised from the upper right first molar (#16) to the upper left second premolar (#25). Buccal bony windows were created between #11 to #13 and #21 to #23. #12 was extracted and the anterior right and left maxillary cysts were fully enucleated with cystic linings intact. Peripheral bone was minimally removed with a bur to gain access for apicoectomy of #22. Apicoectomy of #22 was performed and mineral trioxide aggregate (MTA) retrograde filling was placed. Bio-Gide® membrane (Geistlich Pharma AG, Wolhusen, Switzerland) was used to repair a perforation of the right maxillary sinus membrane.
The eventual cystic defects approximated 1 cm by 1cm on the left and 3 cm by 3 cm on the right. A small round bur was used to create holes along the bony borders of the defects. Two holes were placed on each of the right and left bony borders of the cystic defect at #21 to #23, with the holes approximately 5mm equidistant from one another. This was repeated for the defect at #11 and #12. Three holes were placed on each of the right and left bony borders of the defect at #13 to #15, with all holes approximately 3mm equidistant from one another. 5/0 vicryl sutures were threaded diagonally across the holes, mimicking a shoe-lace pattern to create three separate meshwork (Figure 11).

Tutopatch® membranes (RTI Biologics, TUTOGEN Medical GmbH, Germany) were cut to approximate sizes of the defects, covering 2mm of the bony margins (Figure 12). The membranes were propped up above the meshwork of sutures, and the buccal flap was repositioned and sutured with 5/0 vicryl (Figure 13).

4. Discussion
Various options exist for reconstruction of bone defects after cyst enucleation. This can be done with both bone grafts and a resorbable membrane, with bone graft only or with resorbable membranes only. A systematic review by Buchbender et al. [5] was unable to give an evidence-based clinical recommendation due to low number of studies and data heterogeneity.
Due to possible recurrence of the cyst and risk of post-operative infection, it is not a common and universal practice for placement of bone grafts post-enucleation. In fact, spontaneous bone regeneration can occur even for large cysts, revealing that strengthening of bone with replacement materials may not be required [6]. This simplifies treatment and reduces costs for patients. Rubio et al. [7] reported that mean bone density in defects after spontaneous bone regeneration was approximately 88% of bone density of surrounding healthy bone. Chacko et al. [8] found 100% reduction in size of residual cavity at the end of a 2-year follow-up. These proved that spontaneous osteogenesis after cystic enucleation is feasible.
Furthermore, there is lack of consensus over which filling materials should be used in bone grafting [8]. Filling materials included autogenous bone, platelet-rich plasma and bone substitutes such as hydroxyapatite and β tricalcium phosphate [5]. In large defects where huge volumes of bone grafts are placed, there is also a risk of graft infection and wound dehiscence, complicating post-operative healing.
In the reported cases, large post-enucleation defects were created, making bone grafting impractical. Although spontaneous bone regeneration was likely to occur even without bone grafting, there would have been significant labial bone remodeling and subsequently, labial bone and soft tissue deficiency. This would pose a restorative challenge should anterior teeth be lost in the future. The “shoelace” suture framework was created to support the resorbable membrane and prevent it from collapsing into the hollow cavity. The principle of using a framework to support membranes and maintain its stability has been supported by other studies in the field. Kim et al. [9] described an alternative technique involving an absorbable membrane with a temporary skeletal anchor to increase alveolar width in the anterior mandible. While rigid scaffolding materials can prevent membrane migration, the attendant risks of wound dehiscence, titanium plate exposure and need for secondary retrieval surgery underscore the distinctive advantage of our technique. This novel technique of using resorbable sutures obviates the necessity for a secondary intervention to remove the supporting framework for the membrane and facilitated a guided bone regeneration of the cystic defect, maintaining contour of the labial bone and soft tissue. This is particularly crucial where prosthodontic rehabilitation is considered, as under-contoured and defective soft tissues can compromise on the aesthetic outcomes of prostheses.
Nonetheless, we recognize that long-term studies are required to evaluate the outcomes of hard and soft tissue healing with this approach. This can be done through a prospective study which involves a greater participant pool, coupled with stratification of patients across age cohorts to provide insights into the nuances of healing trajectories. It may also be valuable to evaluate both the quality and quantity of newly formed bone and soft tissues in the region of osseous defect.
5. Conclusion
In conclusion, large bone defects created after enucleation of intra-osseous cystic lesions often result in severe bone and soft tissue deficiency. The “shoelace” sutures are useful to support resorbable membranes used to reconstruct such defects and can potentially reduce the extent of hard and soft tissue deficiency.
Funding
None.
Competing Interests
None.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Celestine Teo and Leonardo Saigo. The first draft of the manuscript was written by Celestine Teo and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Ethics Approval
This study does not require further ethical deliberation because this is a case report for 2 patients. This exemption was granted by SingHealth Centralised Institutional Review Board (CIRB).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent to Publish
The authors affirm that the participants provided informed consent for publication of images in Figures 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12 and 13.
REFERENCES
[1] Nigel
R Johnson, Orla M Gannon, Neil W Savage, et al. “Frequency of odontogenic cysts
and tumors: a systematic review.” J Investig Clin Dent, vol. 5, no. 1,
pp. 9-14, 2014. View at: Publisher
Site | PubMed
[2] M
Spear, P Speight. “Radicular Cyst and Residual Cyst.” In: Cysts of the Oral and
Maxillofacial Regions. Fourth. Blackwell Munksgaard; pp. 123-124, 2007.
[3] R
J Scholl, H M Kellett, D P Neumann, et al. “Cysts and cystic lesions of the
mandible: clinical and radiologic-histopathologic review.” Radiographics,
vol. 19, no. 5, pp. 1107-1124, 1999. View at: Publisher Site | PubMed
[4] Mayara
Santos de Castro, Clenivaldo Alves Caixeta, Marina Lara de Carli, et al.
“Conservative surgical treatments for nonsyndromic odontogenic keratocysts: a
systematic review and meta-analysis.” Clin Oral Investig, vol. 22, no.
5, pp. 2089-2101, 2018. View at: Publisher Site | PubMed
[5] Mayte
Buchbender, Friedrich W Neukam, Rainer Lutz, et al. “Treatment of enucleated
odontogenic jaw cysts: a systematic review.” Oral Surg Oral Med Oral Pathol
Oral Radiol, vol. 125, no. 5, pp. 399-406, 2018. View at: Publisher Site | PubMed
[6] M
Chiapasco, A Rossi, J J Motta, et al. “Spontaneous bone regeneration after
enucleation of large mandibular cysts: a radiographic computed analysis of 27
consecutive cases.” J Oral Maxillofac Surg, vol. 58, no. 9, pp. 942-948,
2000. View at: Publisher Site | PubMed
[7] Eduardo Daniel Rubio, Carlos Mariano Mombrú “Spontaneous Bone Healing after Cysts Enucleation without Bone Grafting Materials: A Randomized Clinical Study.” Craniomaxillofacial Trauma Reconstr, vol. 8, no. 1, pp. 14-22, 2015. View at: Publisher Site | PubMed
[8] Rabin Chacko, Saurabh Kumar, Arun Paul, et al. “Spontaneous Bone Regeneration After Enucleation of Large Jaw Cysts: A Digital Radiographic Analysis of 44 Consecutive Cases.” J Clin Diagn Res, vol. 9, no. 9, ZC84-ZC89, 2015. View at: Publisher Site | PubMed
