Received: Mon 20, Nov 2023
Accepted: Tue 12, Dec 2023
Abstract
Since the 2015 American Thyroid Association Guidelines were released, less total thyroidectomy has been accepted in more patients with differentiated thyroid cancer. The traditional Kocher incision makes it easy to preserve the surrounding structures by securing an adequate surgical field of view, leaving a noticeable postoperative incision scar. Minimally invasive or remote-access extra-cervical approaches have been developed to improve the cosmetic problem. However, considering the high cost, prolonged operation time, and potential morbidity, it isn’t easy to use the alternative-site approaches. A top or necklace may cover an incision scar if the low collar incision is moved to the lateral neck. Therefore, this study evaluated the outcomes of thyroid lobectomy through a lateral collar incision. Seventy-five patients with papillary thyroid carcinoma (PTC) undergoing the lateral collar approach were compared with the non-randomized control of 75 PTC patients undergoing the Kocher incision. The surgical time, bleeding amount, complications, voice, and swallowing function were comparable between this lateral collar and conventional approaches. The cosmetic satisfaction on incision scar was higher than in the traditional incision. The lateral collar approach may be a good alternative for the thyroid lobectomy of PTC. Therefore, this article introduces the procedures and applications of the lateral collar approach as a technical note.
Keywords
Thyroidectomy, incision, lateral collar, cosmetic, surgical approach
Highlights
- Conventional Kocher incision leaves a noticeable postoperative incision scar.
- Minimally invasive or remote-access surgery has been developed to improve the cosmetic problem.
- The approaches may have high costs, prolonged operation time, and potential morbidity.
- A lateral collar incision leads to some cosmetic advantages without increased morbidity.
- This may be an excellent alternative to traditional Kocher or remote-access surgery.
1. Introduction
Traditional thyroid surgery is performed through a collar incision proposed by Emil Theodore Kocher in the late 19th century. Thyroidectomy or parathyroidectomy through a median collar incision has developed to remove one or entire thyroid gland or parathyroid diseases while preserving the recurrent laryngeal nerve and normal parathyroid glands. Open thyroid or parathyroid surgery is currently the most widely used and reliable surgical method, with very low morbidity.
Over the late 20th century, more subclinical lesions were discovered with the development of imaging and aspiration biopsies [1]. With the continuous development of endoscopes and surgical tools, surgical techniques have also been evolved to access areas that are difficult to see with the naked eye and safely remove lesions. Endoscopic surgery made it possible to remove the lesions with smaller incisions and was also used for thyroid and parathyroid surgery [2]. However, no matter how small the incision is in the centre of the lower neck, the incision scar is noticeable after surgery. This might be one of the fears of undergoing thyroid or parathyroid surgery in patients sensitive to scars on the neck and face. This has led to the development of remote-access extra-cervical approaches through the axillar, chest, areolar, retro-auricular, or oral route with more cosmetically favourable outcomes, centring on southeast Asia [3].
Endoscopic and robotic thyroidectomy for the cosmetic advantages requires surgical armamentarium, high cost, and experience to acquire the skill. The alternative incision-site surgery may also increase morbidity and length of hospitalization due to the long and wide flap elevation to access the thyroid or parathyroid glands [4]. Although there are clear cosmetic benefits of incision beyond the neck, the surgical approaches limit these applications to most patients with various thyroid or parathyroid lesions. As an alternative to the cosmetic problem, there has been a suggestion that if a lateral collar incision is made in the supraclavicular area under the side of the neck rather than in the middle, it can be covered by a top or necklace [5]. This may be a good alternative to the traditional Kocher incision, minimally invasive, or remote-access surgery. Therefore, this study evaluated the feasibility and outcomes of thyroid lobectomy through a lateral collar incision. This article also introduces the procedures and applications of thyroid lobectomy through a lateral collar incision.
2. Methods
Most steps in the lateral collar approach are similar to those in the Kocher incision. Before surgery, an incision line was drawn along the natural skin crease on the lower lateral neck of the patient in a sitting position. The patient lies face up with neck extension by placing a shoulder pad under the upper back in a supine position. After sterilizing the neck and covering with surgical drapes, a about 4 cm long lateral collar incision is made along the pre-drawn line on the patient’s neck (Figure 1). A skin flap is lifted along the subplatysmal layer, taking care not to injure the anterior jugular vein. The strap muscles are longitudinally dissected along the median where the left and right meet. The sternohyoid and sternothyroid muscles are laterally retracted to expose the thyroid gland. The superior thyroid artery and vein are separated from the thyroid gland after a sufficient vessel sealing close to the thyroid capsule using bipolar electrocautery or ultrasonic scalpel. The thyroid lobe is dissected from surrounding tissues by attaching it closely to the capsule and pulling it forward with babcock forceps.
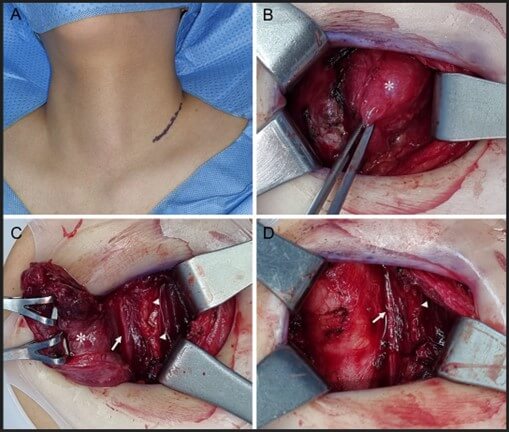
When the tumour slightly infiltrates the strap muscles or other tissues, it is dissected including the surrounding tissues. The superior and inferior parathyroid glands are found and carefully preserved with the supplying vessels after separating from the thyroid gland. The Zuckerkandl’s tubercle growing in the posteromedial margin of the thyroid lobe is found, pulled upwards, and carefully dissected, then discovering and preserving the recurrent laryngeal nerve running along the tracheoesophageal groove without damage. The thyroid lobe is mobilized by careful dissection of berry's ligament from the trachea without damaging the recurrent laryngeal nerve. The thyroid lobe is separated from the remaining thyroid gland with an ultrasonic scalpel.
Pretracheal, prelaryngeal, and ipsilateral paratracheal lymph nodes are simultaneously removed with careful preservation of the superior and inferior parathyroid glands and the recurrent laryngeal nerves. The surgical site is irrigated with saline and haemostasised. The colour of the parathyroid glands is checked, and the gland without viability is chopped and transplanted inside the sternocleidomastoid muscle. Fibrin sealant is sprayed on the surgical field, and the median of the strap muscles is approximated. The skin incision is approximated with absorbable sutures, and tissue adhesive is applied. No drains are inserted, and instead, the operated neck is compressed overnight, and the patient is discharged the following day. The patient is asked to visit the outpatient clinic one week after surgery.
This study involved patients diagnosed with unilateral papillary thyroid carcinoma. Patients with thyroid nodules underwent initial evaluations through ultrasonography and needle biopsies. Only patients undergoing thyroid lobectomy for previously untreated papillary thyroid carcinoma were included in the study. They were then assigned alternately to undergo either the lateral collar approach or the Kocher incision without randomization procedures. The operation site and laryngeal and swallowing functions are checked, cosmetic satisfaction is investigated, and after that, are regularly followed. Pain levels were quantified using a visual analog scale (VAS), with higher scores indicating greater pain intensity. Likewise, evaluations of incision scar aesthetics and cosmetic satisfaction employed VAS scoring, with higher scores indicating increased patient contentment. Patient follow-ups spanned over a minimum of 2 years, with recurrences monitored through physical examinations and imaging studies at outpatient clinics. Ethical approval for this study was obtained from the institutional ethics committee, and informed consent was acquired from each patient.
Continuous variables were expressed as means and standard deviations, while categorical data were presented as numbers and percentages. Statistical differences between the two approaches were determined using the t-test or χ2 test. All tests were two-tailed, and statistical significance was set at P < 0.05 using SPSS 22.0 statistical software (SPSS Inc., Chicago, IL).
3. Results
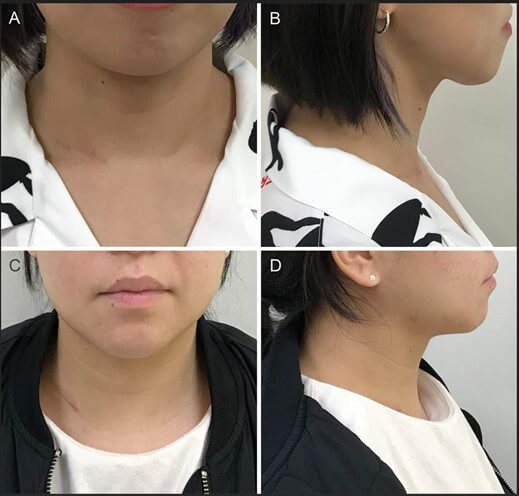
Seventy-five patients experienced successful surgical results through the lateral collar approach. The other 75 patients undergoing the traditional Kocher incision served as the non-randomized control with a comparable distribution of age and sex. Tumors were macroscopically non-invasive and non-metastatic papillary thyroid carcinomas only located in the ipsilateral lobe with a median size of 1.6 cm (0.8-3.4 cm) comparable between the two approaches. The median operation time was 62 min vs. 58 min, and the median blood loss was 25 mL vs. 22 mL (P > 0.1). Only one patient experienced temporary vocal cord paralysis in the conventional group. None of the patients in both groups had any early complications, such as hematoma, dyspnea, and swallowing difficulties, and all were safely discharged the day after surgery. The median score of postoperative pain sensation was 3 of the 10-point visual analogue scales in both groups. Median patient's cosmetic satisfaction in the 6th postoperative month was 8 in the lateral approach and 4 in the conventional approach (P < 0.01) (Figure 2). One nodal recurrence was found in the lateral neck of the traditional group for the median follow-up of 44 months (24-60 months).
4. Discussion
The present investigation underscores the effectiveness of the lateral collar approach in managing unilobe-localized papillary thyroid carcinomas, manifesting commendable outcomes concerning aesthetics, minimal adverse events, and a notable absence of recurrences. Napolitano et al. first introduced that 1165 thyroid and parathyroid patients were successfully operated on without complications using the lateral approach technique in 1997 [5]. Henry and Sebag also reported a lateral endoscopic approach to remove the thyroid lobe or parathyroid glands by directly accessing the posterior aspect of the thyroid gland [6]. Afterward, there have been several reports on the cosmetic advantages of the lateral approach compared to the conventional collar incision. Chen et al. reported that when one thyroid lobe was removed through a lateral collar incision with an average of 5.2 cm (range 3 to 8 cm) in 98 patients, an average cosmetic satisfaction score of 8.7 was obtained without any increase in complications [7].
Ren et al. showed lower pain and higher cosmetic satisfaction in the lateral incision group with no difference in operation time, bleeding amount, morbidity, and hospital stay when comparing the results of 90 patients with unilateral papillary thyroid carcinoma each using lateral and conventional collar incisions [8]. Dissanayake et al. suggested that the lateral collar approach was helpful in redoing thyroid surgery as it was safe without any increase in complications as the results of this approach in a total of 36 patients, including 9 reoperation patients [9]. There may also be no difficulty in securing the surgical field with this approach when performing ipsilateral central lymph node dissection. These findings serve to further validate the practicality of the lateral collar approach as a valuable strategy in the context of unilateral thyroid tumors.
The lateral collar approach may be applied to unilateral thyroid benign or atypical lesions that may require surgery and unilateral differentiated thyroid cancer less than 4 cm without significant invasion into surrounding tissues. This approach does not apply to patients with bilateral thyroid cancer or thyroid lesions requiring surgery. This may also be relatively limited or difficult in the cases of thyroid cancer with gross invasion, clinical lymph node metastasis, a history of radiation therapy, and severe thyroiditis. The indications of the lateral collar approach are not limited compared to the remote-access approaches. This surgery can be performed with a similar operating time to the conventional collar incision in a wider and well-secured field of view for checking surrounding structures.
This study confirmed the feasibility and reliable outcomes of the lateral collar approach. The limitations of this study are no comparisons with other cosmetic approaches. Further studies are needed to validate the long-term outcomes and compare the morbidities and results with conventional Kocher incision and remote access approaches. Since the 2015 American Thyroid Association Guidelines were released, minimally invasive or remote-access thyroid surgery has received more attention as the number of patients applying for unilateral thyroid lobectomy increases [3]. In modern thyroid surgery, it is difficult to argue that one approach is the best, and as the saying goes, “One size does not fit all,” it can be essential to select patients who need each approach [10].
5. Conclusion
Given the pros and cons of several surgical approaches, the lateral collar approach, with some cosmetic advantages, may be an excellent alternative to the extravagant remote-access techniques in an era of de-escalation thyroid surgery. It will be necessary to prove its usefulness through future comparative studies with other cosmetic considering approaches.
Author Contributions
Jong-Lyel Roh: Conception and design of the study, data acquisition, analysis and interpretation of data, drafting the manuscript, and accountable for all aspects of the work.
Conflicts of Interest
None.
REFERENCES
[1] Lindsey Enewold, Kangmin Zhu, Elaine
Ron, et al. “Rising thyroid cancer incidence in the United States by
demographic and tumor characteristics, 1980-2005.” Cancer Epidemiol
Biomarkers Prev, vol. 18, no. 3, pp. 784-791, 2009. View at: Publisher Site | PubMed
[2] P Miccoli, P Berti, M Conte, et al.
“Minimally invasive surgery for thyroid small nodules: preliminary report.” J
Endocrinol Invest, vol. 22, no. 11, pp. 849-851, 1999. View at: Publisher Site | PubMed
[3] Jonathon O Russell, Salem I
Noureldine, Mai G Al Khadem, et al. “Minimally invasive and remote-access
thyroid surgery in the era of the 2015 American Thyroid Association
guidelines.” Laryngoscope Investig Otolaryngol, vol. 1, no. 6, pp.
175-179, 2016. View at: Publisher
Site | PubMed
[4] Kyung Tae, Yong Bae Ji, Chang Myeon
Song, et al. “Robotic and endoscopic thyroid surgery: Evolution and advances.” Clin
Exp Otorhinolaryngol, vol. 12, no.1, pp. 1-11, 2019. View at: Publisher Site | PubMed
[5] C Napolitano, M Vix, D Mutter, et al.
“Thyroid and parathyroid surgery: is the medial approach truly elective?
Technique and advantage of the lateral approach.” Minerva Chir, vol. 52,
no. 11, pp. 1393-1395, 1997. View at: PubMed
[6] J-F Henry, F Sebag “Lateral
endoscopic approach for thyroid and parathyroid surgery”. Ann Chir, vol.
131, no. 1, pp. 51-56, 2006. View at: Publisher Site | PubMed
[7] Zhi-qiang Chen, Lei Wang, Tao Li, et
al. “Supraclavicular lateral collar incision versus conventional approach for
thyroidectomy: supplement for minimally invasive techniques with extended
indications.” J Laparoendosc Adv Surg Tech A, vol. 21, no. 1, pp. 45-50,
2011. View at: Publisher
Site | PubMed
[8] Yan-Xin Ren, Jie Yang, Wei-Ze Sun, et
al. “Application of lateral supraclavicular incision in unilateral thyroid
papillary carcinoma surgery.” Braz J Otorhinolaryngol, vol. 88 no. Suppl
1, pp. S42-S47, 2021. View at: Publisher Site | PubMed
[9] Duminda DMC Dissanayake, Ranil F Fernando, Iresha J Dissanayake “Lateral approach to thyroid: A good technique for reoperative thyroid surgery.” World J Endoc Surg vol. 8, no. 2, pp. 141-142, 2016. View at: Publisher Site
[10] David J Terris “Surgical approaches to the thyroid gland: which is the best for you and your patient?” JAMA Otolaryngol Head Neck Surg, vol. 139, no. 5, pp. 515-517. View at: Publisher Site | PubMed
