Received: Fri 26, Jan 2024
Accepted: Mon 19, Feb 2024
Keywords
Pelvis, membrane anatomy, terminology, consensus
1. Introduction
Total mesorectal excision (TME) proposes the concept of membrane anatomy-guided surgery, which changes the traditional view that surgical dissection focuses on organs or blood vessels, and has led to the development of third-generation surgical anatomy, “membrane anatomy”. Membrane anatomy mainly studies various membrane structures of the abdominopelvic cavity related to surgery, such as peritoneum, mesentery, fascia, serosa, and their derived ligament, lamina, septum, bundle, space, sheath, etc. In clinical practice, membrane anatomy emphasizes that the complete excision of the organ-specific mesentery is conducted through the membrane anatomical plane, which can significantly reduce bleeding and ensure the integrity of the mesentery. Due to the rapid development of the theory and practice of membrane anatomy, it is urgent to revise and update the existing terms for more standardized and reasonable use. Published in 1998 by the Federative Committee on Anatomical Terminology (FCAT), Terminologia Anatomica presents the international reference standard of anatomic terms. However, Terminologia Anatomica only assigns anatomical terminology to the pelvic connective tissue bundle covered with the peritoneum and lacks definitions for the connective tissue planes and space used in surgical practice [1, 2]. Moreover, pelvic anatomy involves many disciplines in clinical practice, such as urology, gynecology, and colorectal surgery. Each discipline has its anatomical term, which easily leads to different terms being used for a single structure. With the development of anatomy, many definitions of membrane anatomical terms have changed and new terms have appeared. Because of this, the Chinese Society of Colorectal Surgery (CNSCRS) organized experts to create a standardized list of preferred terminology for pelvic membrane anatomy to be used in medical communication.
2. Methodology
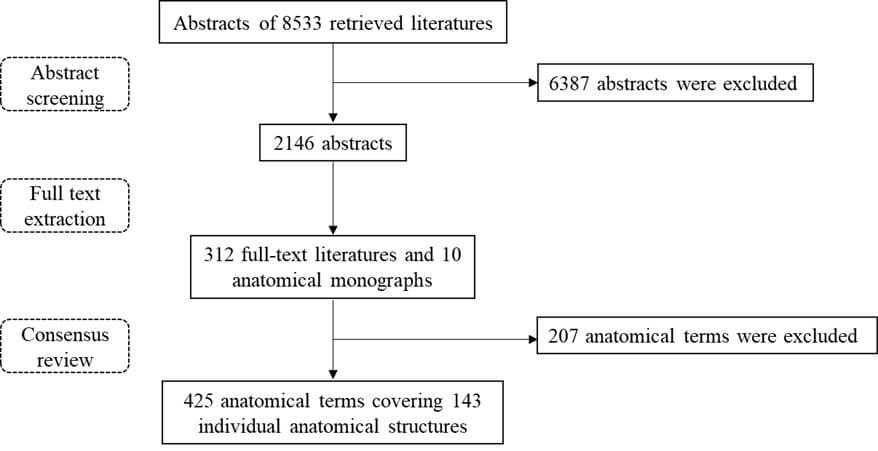
The Consensus Drafting Group included colorectal, urologic, and gynecologic surgeons with extensive clinical, anatomic, surgical, and imaging expertise and statisticians with experience in systematic review methodologies. First, the Medline database was searched from inception until December 31, 2022, based on the following 17 medical subject heading terms: pelvis, mesentery, mesorectum, mesometrium, fascia, peritoneum, serosa, ligament, lamina, bundle, tendon, sheath, septum, space, fossa, layer, plane. The obtained abstracts were screened by five researchers using the online software Abstrackr (Link). The included literature was mainly related to cadaveric anatomy, surgery, and pelvic imaging, and literature dealing with anatomical variations, histology, and biomechanics was excluded. Finally, 6387 abstracts were excluded, and the remaining 2146 abstracts were further screened by full-text extraction, and 312 full-text literatures were obtained. To ensure that the selected anatomical terms are more representative, 10 classic anatomical monographs were added by group consensus [3-12]. The group reviewed 312 full-text documents and 10 anatomical monographs, obtaining 632 anatomical terms, 207 of which were excluded because they were not relevant or representative of pelvic membrane anatomy, and finally retained 425 membrane anatomical terms covering 143 independent anatomical structures (Figure 1).
For the final list of anatomic terms, all terms with an exact reference in Terminologia Anatomica were accepted. The remaining identified terms were discussed until group consensus was obtained on which terms to recommend for use based on the frequency of occurrence in the literature. The initial findings were presented at the 16th annual meeting of the Chinese College of Surgeons (CCS) in July 2017 in Shanghai. The list of terms, definitions, and key references was then distributed to 79 experts across 33 different cities and 71 hospitals for review and confirmed by secret voting using an electronic program. Consensus was established as 75% agreement among the participating experts on the definition of each term.
3. Recommended Terms of Pelvic Membrane Anatomy
The elucidation of each term includes the identification number in Terminologia Anatomica if it has, synonym (different names appeared in the literature), and definition (the widely accepted concepts previously).
3.1 Generic Terms
3.1.1. Visceral Pelvic Fascia (A04.5.03.002)
3.1.1.1. Synonym
Visceral layer of the pelvic fascia [13], fascia pelvis visceralis [14].
3.1.1.2. Definition
The visceral pelvic fascia is a generic term for the fascia which lies immediately outside the visceral layer of the serosae together with that which immediately surrounds the viscera [3, 5, 10, 12].
3.1.1.3. Annotation
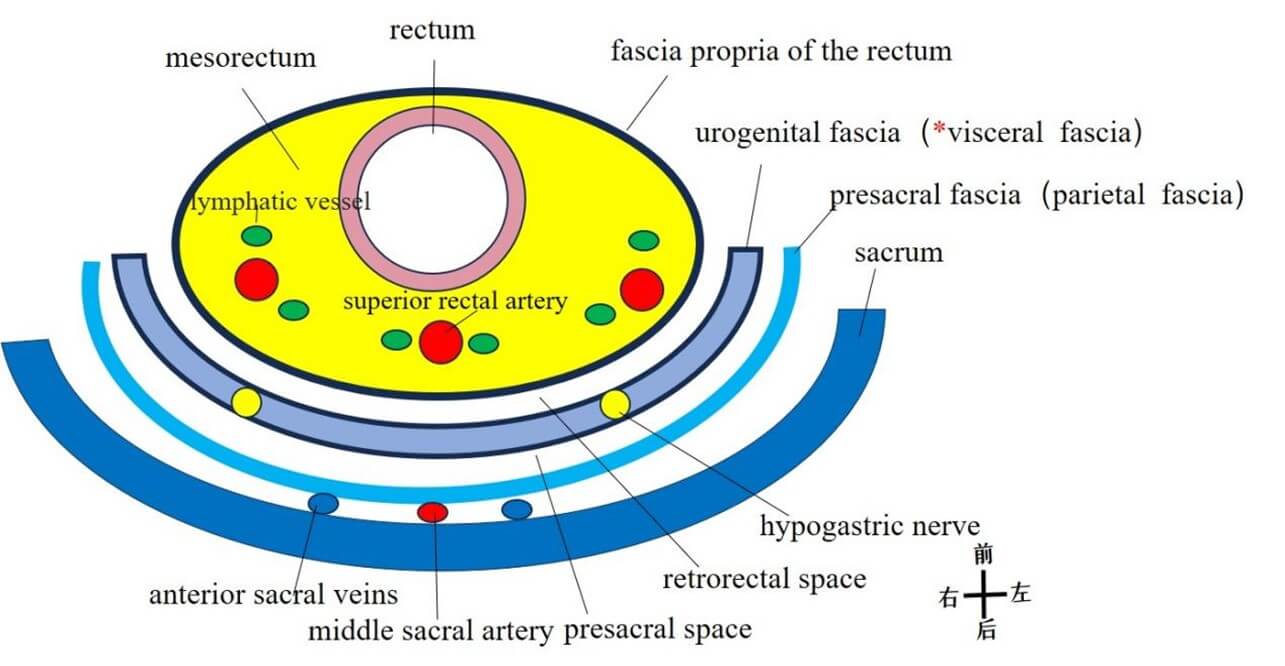
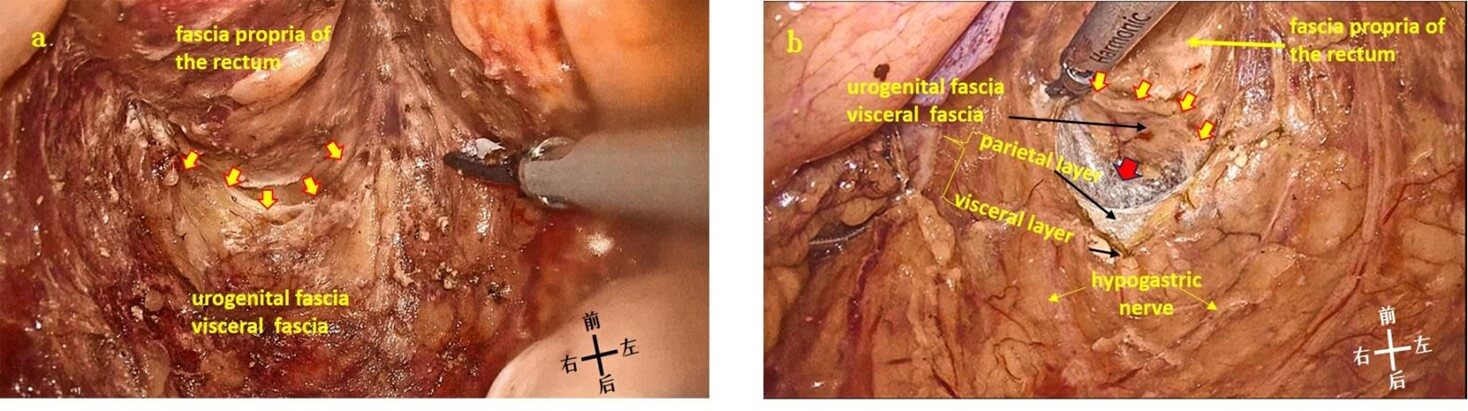
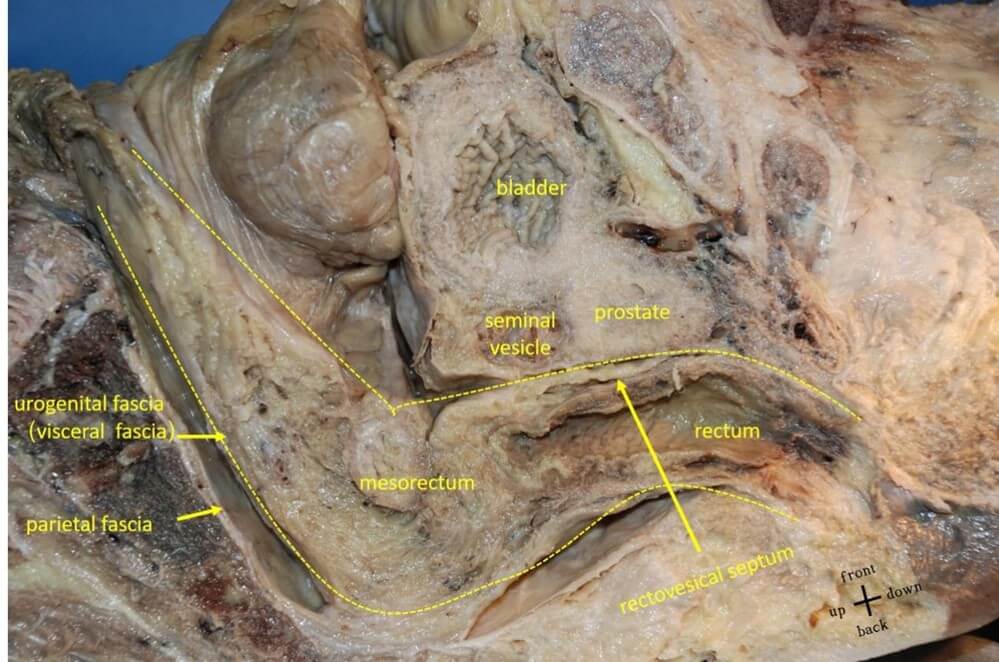
There are three different layers of viscera fascia: i) The fasciae surrounding individual organs. ii) The septum between organs. iii) The sheath or ligament that connects organs to the pelvic wall (neurovascular sheath) [10, 15]. However, the clinically accepted definition of visceral pelvic fascia has changed since the introduction of total mesorectal excision (TME) in clinical practice. It refers specifically to a dense layer of fascia posterolateral to the rectum, and the mesorectum is enveloped by the visceral fascia (Figure 2) [16-18].
3.1.1.4. Recommendation 1
Visceral pelvic fascia is a generic anatomical term and can be defined as the fascial system originating in the reflection of the parietal pelvic fascia, which envelops the individual organs and attaches them to the pelvic walls. The term "visceral fascia" should be avoided to refer to specific pelvic fascia such as the mesorectal fascia. Approval rate: 98.6% (70/71).
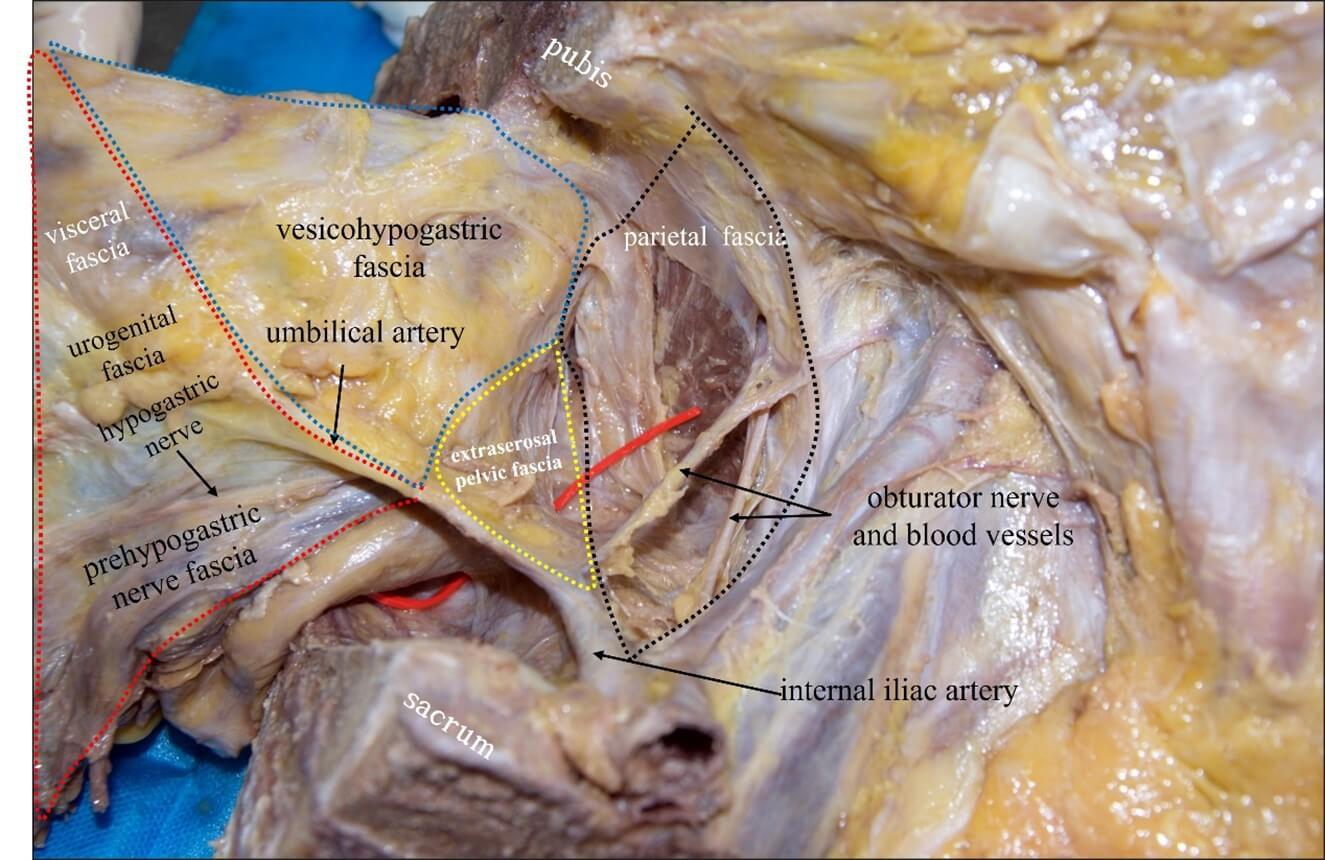
The red dotted line is the visceral fascia (urogenital fascia) according to classic anatomy [16]. The blue dotted line is the vesicohypogastric fascia. The black dotted line is the parietal fascia. The yellow dotted line is the extraserosal fascia.
3.1.2. Parietal Pelvic Fascia (A04.5.03.007)
3.1.2.1. Synonym
Endopelvic fascia [1], fascia pelvis parietalis [14].
3.1.2.2. Definition
The parietal pelvic fascia is the fascia that extends from the endoabdominal fascia and covers the inner surface of the pelvic parietal muscles and bones. It can be divided into four parts: the superior fascia of the pelvic diaphragm, piriformis fascia, obturator fascia, and presacral fascia [6, 10, 12, 19-21]. The parietal fascia is locally thickened to form a tendinous arch or ligament, such as the tendinous arch of pelvic fascia, the tendinous arch of the levator ani, the tendinous arch of rectovaginal fascia, and the pubovesical ligament [7, 22].
3.1.2.3. Annotation
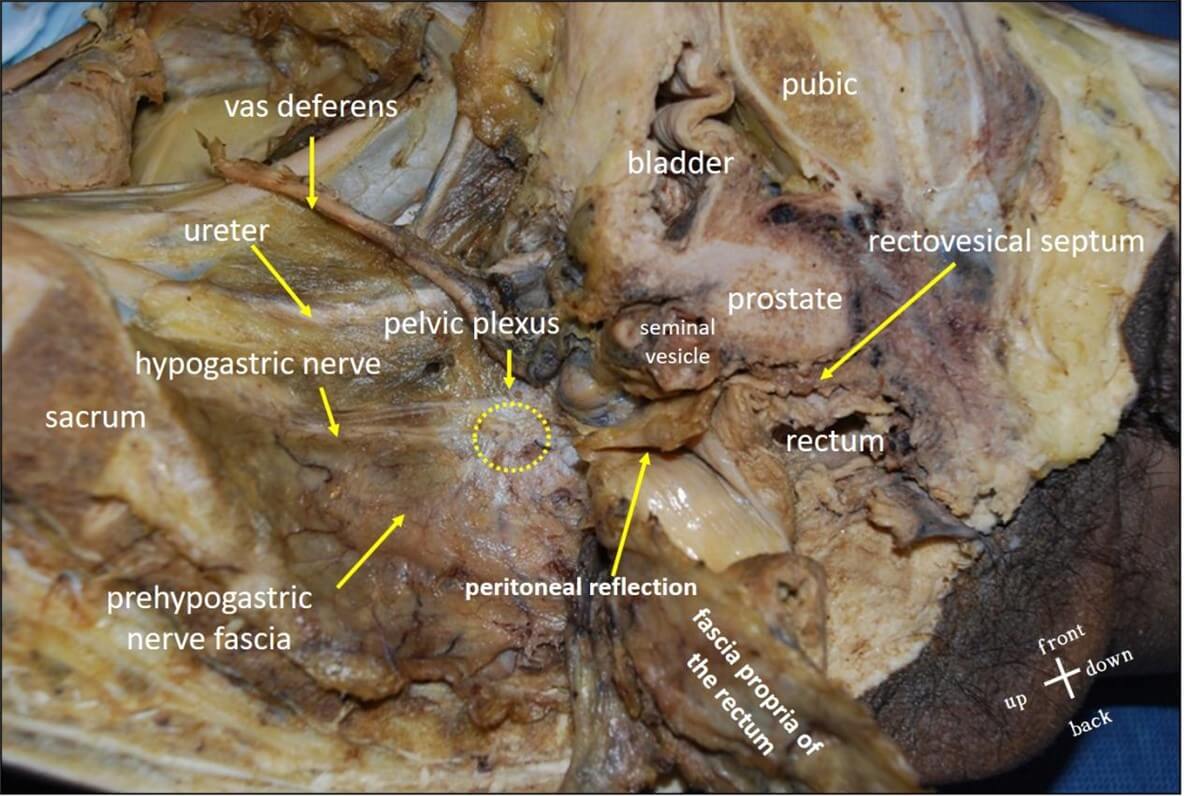
The fasciae covering the surface of the diaphragm, psoas major, quadrate psoas, and transverse abdominis are collectively referred to as the endo abdominal fascia or the transversal fascia in a general sense [23]. Two anatomical views on the parietal fascia are questionable. First, the Japanese anatomical literature divides the subperitoneal fascia into the deep layer (anterior renal fascia or Gerota’s fascia) and the superficial layer (posterior renal fascia or Gerota’s fascia), and are called visceral fascia and parietal fascia respectively when extending to the pelvic cavity [17, 24]. This view is contradicted by the viewpoint that the parietal pelvic fascia continues from the endo abdominal fascia or the transversalis fascia. Second, the parietal pelvic fascia is divided into two layers and encloses the autonomic nerve such as the hypogastric nerve according to Western perspectives [25-27]. This view confuses the definitions between visceral and parietal fascia because the fascia constituting the neurovascular channels belongs to visceral fascia according to Recommendation 1 (Figure 3).
3.1.2.4. Recommendation 2
The parietal pelvic fascia covers the pelvic walls, and consists of four parts: superior fascia of the pelvic diaphragm, piriformis fascia, obturator fascia, and presacral fascia. Approval rate: 100.0% (71/71).

3.1.3. Endopelvic Fascia (A04.5.03.007)
3.1.3.1. Synonym(s)
Extraserosal pelvic fascia [22].
3.1.3.2. Definition
The pelvic visceral fascia and parietal fascia are collectively called endopelvic fascia [14, 21, 28].
3.1.3.3. Annotation
The description of endopelvic fascia is fairly standardized. Terminologia Anatomica identifies it as parietal fascia [1]. Hollinshead [10] believed that endopelvic fascia belongs to visceral fascia. Grant's Atlas of Anatomy called the connective tissue between the visceral and parietal fascia endopelvic fascia. The endopelvic fascia is composed of loose and condensed parts. The loose part is the fat tissue filled in the potential space. The dense part constitutes the neurovascular channel between the organs and the pelvic side wall [3, 6, 8], which is consistent with the definition of extraserosal fascia proposed by Ercoli et al. [22] (Figure 2). However, the neurovascular sheath belongs to the visceral fascia in a strict sense. In recent years, it is more inclined to regard the endopelvic fascia as a general term of visceral and parietal fascia, and it is believed that all the fascia or ligaments of different densities in the pelvic cavity are parts of the endopelvic fascia [14, 21, 28]. (Figure 2).
3.1.3.4. Recommendation 3
The endopelvic fascia is a general term for pelvic visceral fascia and pelvic parietal fascia. It is recommended to use parietal endopelvic fascia and visceral endopelvic fascia to distinguish them. Approval rate: 97.2% (69/71).
3.2. Specialized Anatomical Terms
3.2.1. Terms Related to Visceral Fascia
3.2.1.1 Fasciae of Organs
3.2.1.1.1. Fascia of the Individual Organ (A04.5.02.003)
3.2.1.1.1.1. Synonym(s)
None.
3.2.1.1.1.2. Definition
The proper fascia of pelvic organs [1].
3.2.1.1.1.3. Annotation
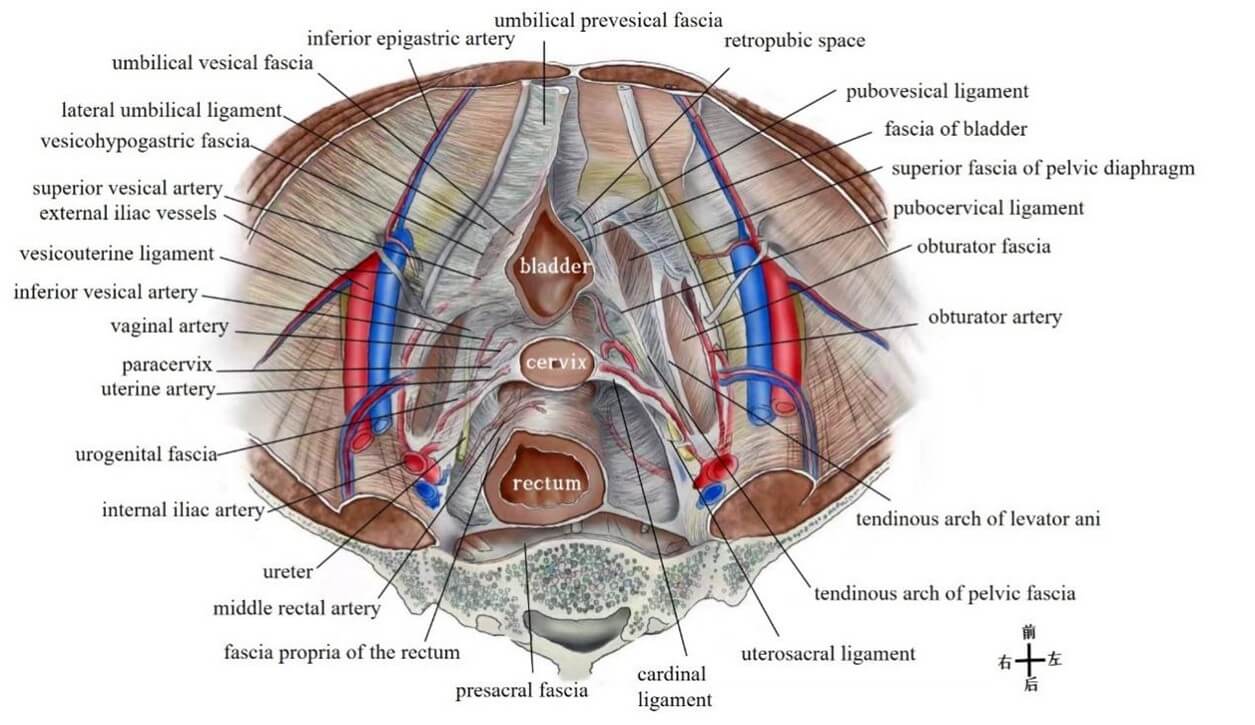
Fascia of individual organ is part of the visceral fascia, which can be specifically divided into vesical fascia, rectal fascia, and vaginal fascia [15, 22] (Figure 4).
3.2.1.1.2. Fascia Propria of the Rectum
3.2.1.1.2.1. Synonym(s)
Mesorectal fascia [29], perirectal fascia [30], rectal fascia [31], visceral fascia [16].
3.2.1.1.2.2. Definition
The innermost layer of fibrous connective tissue surrounding the mesorectum is called the fascia propria of the rectum [32, 33].
3.2.1.1.2.3. Annotation
The fascia propria of the rectum is more pronounced anterior to the rectum because it contains less fat, and sometimes is referred to as the posterior layer of Denonvilliers’ fascia [10, 34]. The fascia propria of the rectum is always thought to be part of the visceral fascia, which wraps the rectum to form the mesorectum, so the plane between the visceral and parietal fascia constitutes the "Holy plane" of rectal cancer surgery [16, 18, 35]. Recent studies have suggested that fascia propria of the rectum and "visceral fascia" described by Heald et al. [16] are two independent layers of fascia, but they fuse at the level of S2~S4, and the fusion line is not fixed (Figures 5 & 6) [32, 36].
3.2.1.1.2.4. Recommendation 4
In terms of the fascial continuity, the colonic fascia surrounding the mesocolon is in continuity with the fascia propria of the rectum enveloping the mesorectum in the pelvis. The anterior and posterior renal fascia extending into the pelvic cavity is called urogenital fascia which is actually the "visceral fascia" described by Heald et al. Therefore, visceral fascia and the fascia propria of the rectum are two independent layers of fascia. Approval rate: 97.2% (69/71).
3.2.1.2. Septum between Organs
3.2.1.2.1. Rectovesical Septum (A04.5.03.004), Rectovaginal Septum (Rectovaginal Septum, A04.5.03.004)
3.2.1.2.1.1. Synonym(s)
Denonvilliers' fascia [37], rectovaginal fascia [21], peritoneoperineal fascia [11], rectogenital fascia [38], prostatoseminal vesicular fascia [39], prostatoperitoneal membrane [40].
3.2.1.2.1.2. Definition
The rectovesical septum lies between the rectum and the prostate /seminal vesicle, while the rectovaginal septum lies between the rectum and the vagina [3]. The rectovesical (vaginal) septum passes from the peritoneum of the rectovesical (vaginal) pouch above to the pelvic floor in the region of the perineal body below [20].
3.2.1.2.1.3. Annotation
According to the Nomina Anatomica, personal names cannot be used to name anatomical structures, so "Denonvilliers fascia" cannot be used as a standard anatomical term [1]. The rectovesical (vaginal) is obvious in males but hardly is identifiable in females. The appearance varies considerably, from a fragile translucent layer to a tough leathery membrane [41]. There is still controversy as to whether the rectovesical (vaginal) septum is a single or double layered structure. At present, it is widely recognized as a single-layer structure, and the posterior layer is the fascia propria of the rectum (Figure 7) [34, 42, 43].
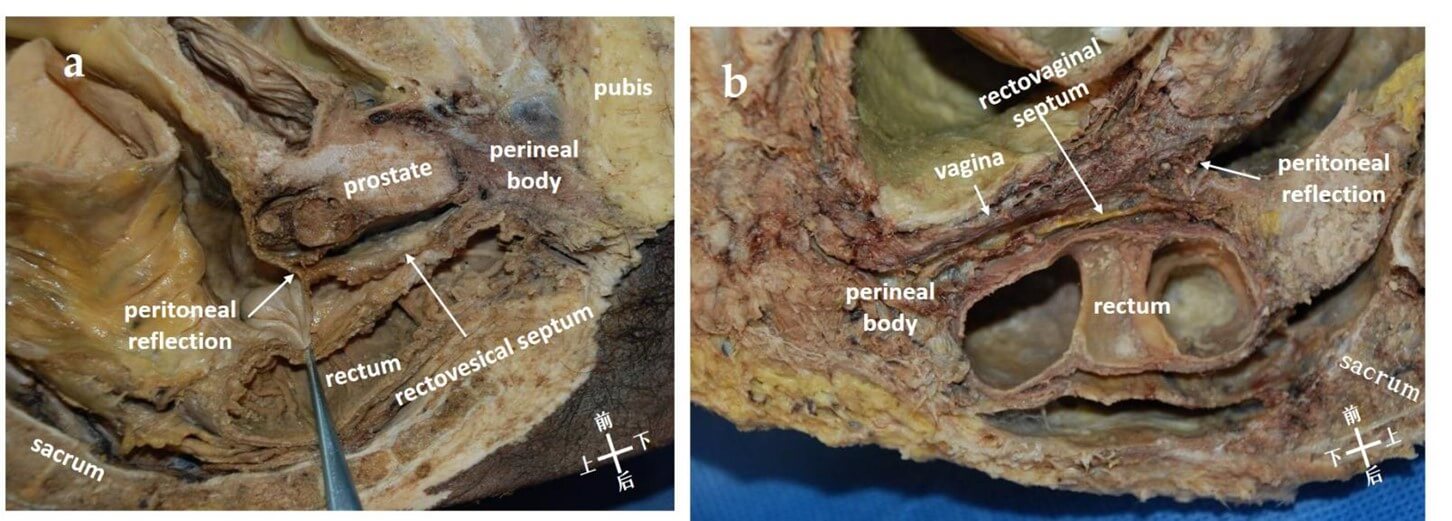
3.2.1.2.1.4. Recommendation 5
It is recommended to use the rectovesical septum or rectovaginal septum instead of Denonvillliers' fascia, and to avoid referring to the fascia propria of the rectum as the posterior layer of Denonvillliers' fascia. Approval rate: 85.9% (61/71).
3.2.1.2.2. Pubovesical Ligament (A04.5.03.013)
3.2.1.2.2.1. Synonym
Pubourethral Ligament [5], puboprostatic ligament [5].
3.2.1.2.2.2. Definition
The pubovesical ligament extends from the bladder neck to the inferior aspect of the pubic bone [8, 44]. The dorsal vein complex (DVC), also known as the Santorini plexus, passes between the paired pubovesical ligaments [45].
3.2.1.2.2.3. Annotation
This ligament is called the pubovesical ligament in females and the puboprostatic ligament in males [5]. Although this term is commonly used, the pubourethral ligament is questioned as a different structure than the tendinous arch of pelvic fascia [6, 22, 46]. Due to the ligament containing smooth muscle derived from the bladder, it is also thought to be part of the detrusor apron (Figure 4) [38, 45].
3.2.1.2.3. Pubocervical Ligament (A09.1.03.030)
3.2.1.2.3.1. Synonym(s)
Pubocervical fascia [21].
3.2.1.2.3.2. Definition
The pubocervical ligament originates from the pubic symphysis and attaches to the cervix and upper vagina [3].
3.2.1.2.3.3. Annotation
Classical anatomical literature including Gray's Anatomy (41st edition) considers the pubocervical ligament to be an exact anatomical structure formed by thickened pelvic fascia [3]. Since its alignment with the pelvic fascia tendon arch, it has been suggested that the pubocervical ligament is part of the pelvic fascial tendon arch and is located between the pelvic fascial tendon arch and the lateral wall of the middle and lower 1/3 of the vagina [22]. However, it has also been suggested that the pubocervical ligament is the vesicouterine ligament (Figure 4) [47].
3.2.1.2.4. Vesicouterine Ligament
3.2.1.2.4.1. Synonym
Anterior parametrium [48], bladder pillar [49], vesicovaginal ligament [50], vesicocervical ligament [51], vesicocervical pillar [51], vesicovaginal pillar [51], Amreich's fleboduct [22].
3.2.1.2.4.2. Definition
The vesicouterine ligament is formed by the extension of both sides of the uterine tissue to the ventral side and surrounding the blood vessels, nerves, and distal ureter, and is located above and beneath the ureter to form a "ureteral tunnel" [48, 52, 53].
3.2.1.2.4.3. Annotation
The vesicovaginal ligament can be divided into deep and superficial layers, or anterior and posterior lobes, bounded by the ureter. There are also literature that refer to the superficial layer as the vesicovaginal ligament and the deep layer as the vesicovaginal ligament [53]. The superficial layer of the vesico-uterine ligament forms the top of the ureteral tunnel and covers the ureter above the layer of connective tissue between the cervix and the bladder, which contains the cervico-vesical vessels from the uterine artery. The deep (posterior) layer of the vesicouterine ligament is located beneath the ureter and is the connective tissue connecting the posterior wall of the bladder with the cervix and the lateral side of the upper vagina. The veins and nerves of the bladder run along it (Figures 4, 8 & 9) [54].
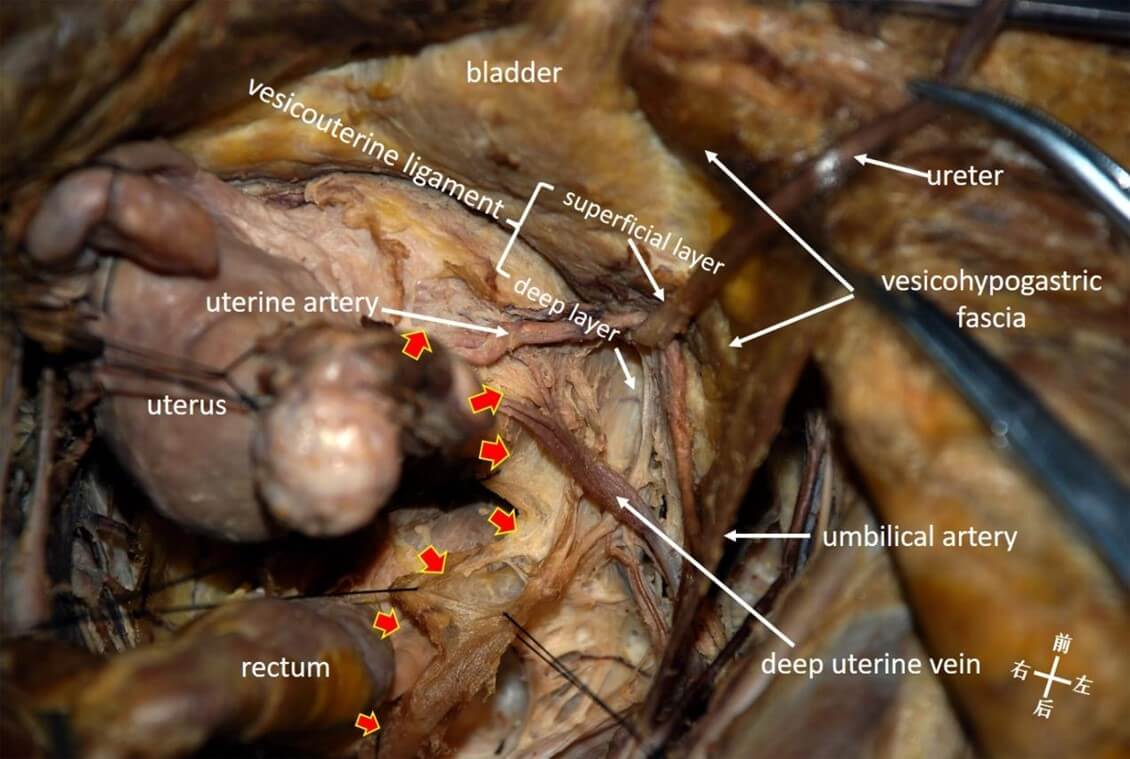
3.2.1.2.4.4. Recommendation 6
The vesicouterine ligament is a connective tissue containing nerves and blood vessels located between the end of the ureter, the urogenital fascia, and the vesicohypogastric fascia. It is divided into a superficial layer and a deep layer by the ureter. Voting approval rate: 98.6% (70/71).
3.2.1.2.5 Uterosacral Ligament (A09.1.03.032)
3.2.1.2.5.1. Synonym(s)
Rectouterine ligament [55], rectovaginal ligament [55], sacrouterine ligaments [56], posterior parametrium [57].
3.2.1.2.5.2. Definition
The uterosacral ligaments emanate from the cervix and the corpus uteri and are attached to the front of the sacrum through both sides of the rectum [3, 4].
3.2.1.2.5.3. Annotation
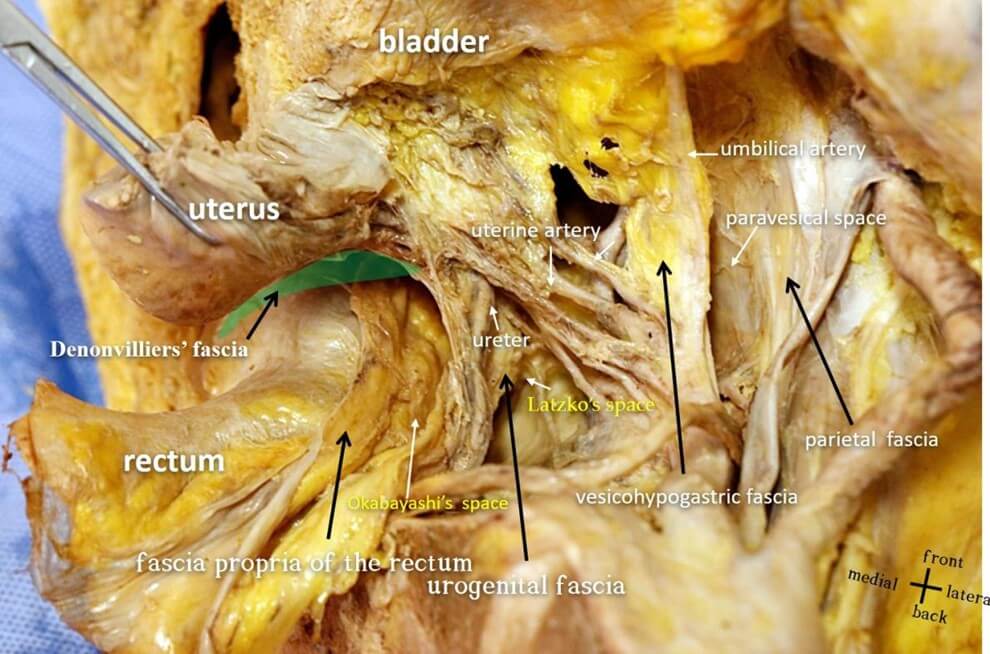
The uterosacral ligament consists of three parts: recto-uterine fold, rectouterine ligament, and rectovaginal ligament [58]. The anatomic feature of the uterosacral ligament is that it has a hypogastric nerve and pelvic nerve plexus on the external side [55, 59] and is not directly attached to the sacrum [60], which is consistent with the anatomic feature of the urogenital fascia (Figures 8 & 10) [61].
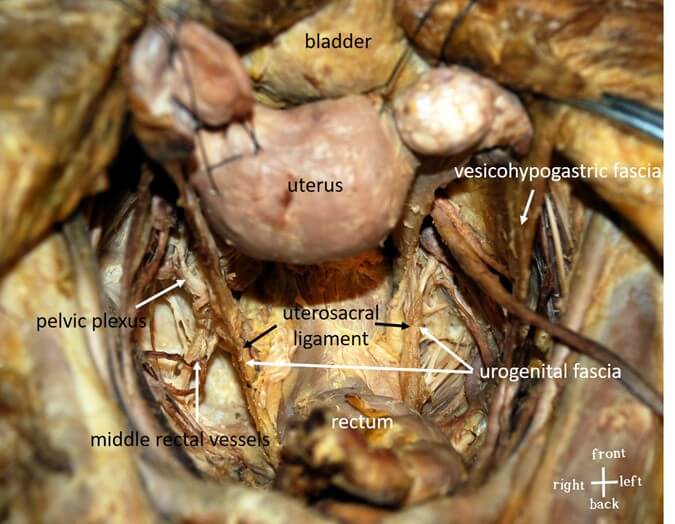
3.2.1.2.5.4. Recommendation 7
The uterosacral ligament is a part of the urogenital fascia located between the anterior sacral and the uterus. Voting approval rate: 100.0% (71/71).
3.2.1.2.6. Rectosacral Fascia (A04.5.03.019)
3.2.1.2.6.1. Synonyms
Presacral fascia [16], Waldeyer's fascia [16], posterior parametrium [62].
3.2.1.2.6.2. Definition
The recto sacral fascia originates from the anterior sacral fascia and extends forward and downward to join the fascia propria of the rectum. The starting point of the recto sacral fascia is not constant, but it is located in S2~S4, and theendpointt is generally 3-5 cm above the anorectal junction [3].
3.2.1.2.6.3. Annotation
Some studies have suggested that the rectosacral fascia is formed by the fusion of the anterior fascia of the hypogastric nerve and the fascia propria of the rectum at the level of S2-S4 sacrum [63], but in fact, the rectosacral fascia starts from the anterior sacral fascia (parietal fascia), runs diagonally upward, crosses the urogenital fascia (visceral fascia), and ends at the fascia propria of the rectum [61]. Anatomically, the rectosacral fascia appears as a continuation of the urogenital fascia. Some studies refer to the rectosacral fascia (ligaments) as Waldeyer fascia [64-66], or the entire anterior sacral fascia as Waldeyer fascia [16, 31]. However, in Waldeyer's book Das Becken (The Pelvis), no fascial structure is described between the rectum and the sacrum, and the fascia named after Waldeyer does not exist [64]. At present, Waldeyer fascia is mostly described as formed by the fusion of the distal end of the anterior sacral fascia and the fascia propria of the rectum at the anorectal junction (Figure 11) [67-70].
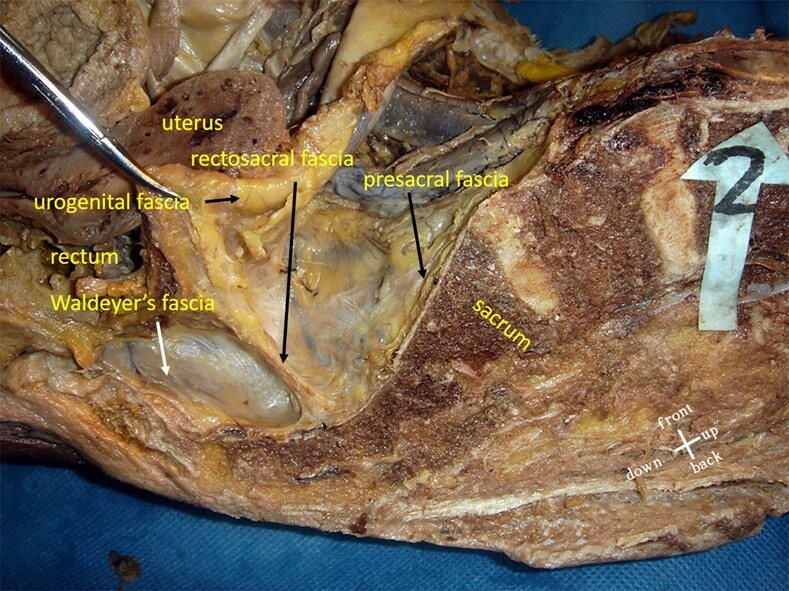
3.2.1.2.6.4. Recommendation 8
The presacral fascia, rectosacral fascia, and Waldeyer's fascia are three different anatomical structures. The presacral fascia is the thickened part of the presacral wall fascia, while the rectosacral fascia connects the presacral fascia and the rectal intrinsic fascia at the S2-S4 sacral level, dividing the retrorectal space into upper and lower compartments. Given the ambiguous definition of Waldeyer’s fascia and its lack of specific clinical anatomical relevance, it is recommended to discard the use of Waldeyer's fascia as an anatomical term. Voting approval rate: 95.8% (68/71).
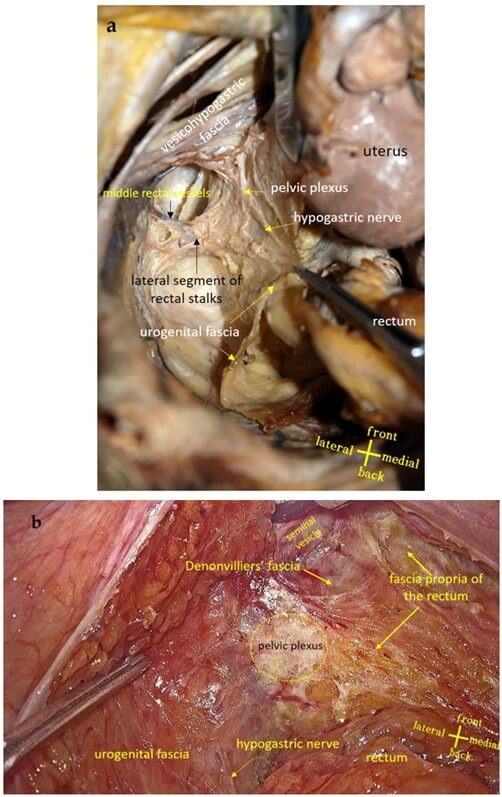
3.2.1.2.7. Urogenital Fascia
3.2.1.2.7.1. Synonym(s)
Ureteral sheath [71], periureteric fascia [71], perirenal fascia [72], hypogastric nerve sheath [31], ureterohypogastric fascia [73], urogenital-hypogastric sheath [74], hypogastric nerve fascia [75], urogenital sheath [75], urogenital stratum [76], sacro-recto-genitopubic lamina [77], intermediate stratum of the retroperitoneal tissue [72], ureteroneural lamina [78].
3.2.1.2.7.2. Definition
The urogenital fascia continues from the anterior and posterior renal fascia, comprising the connective tissue sheath that contains the ureter, genital vessels, and hypogastric nerve [31, 77].
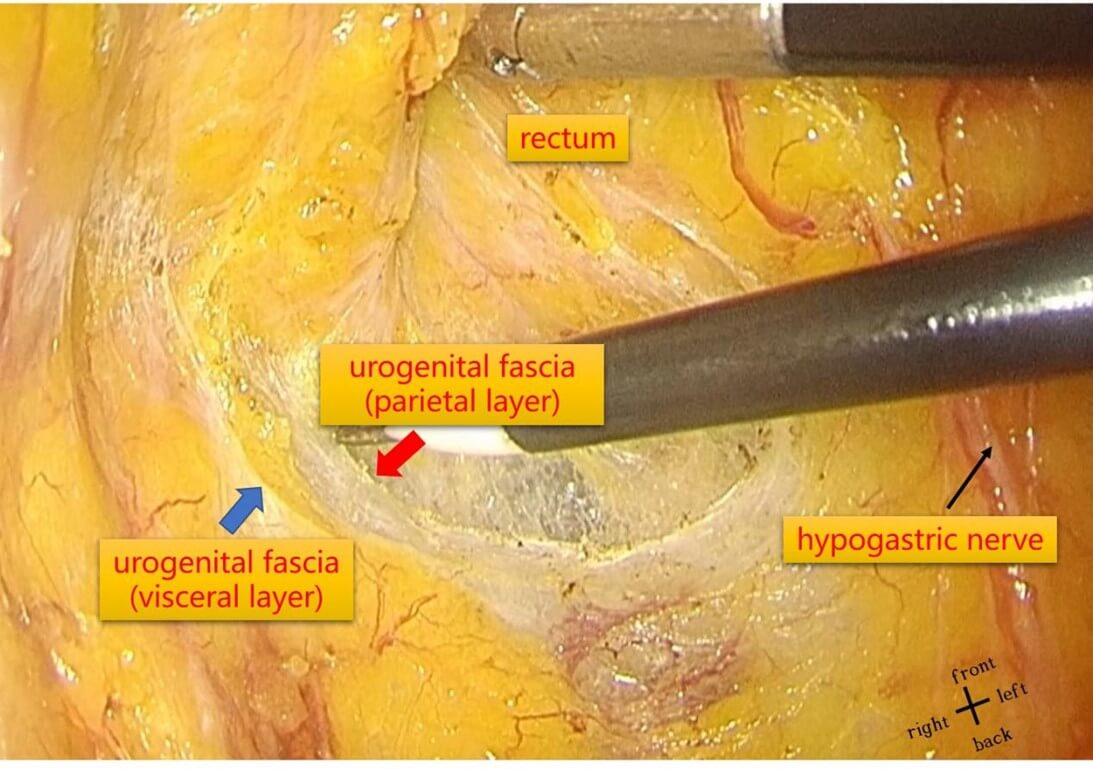
3.2.1.2.7.3. Annotation
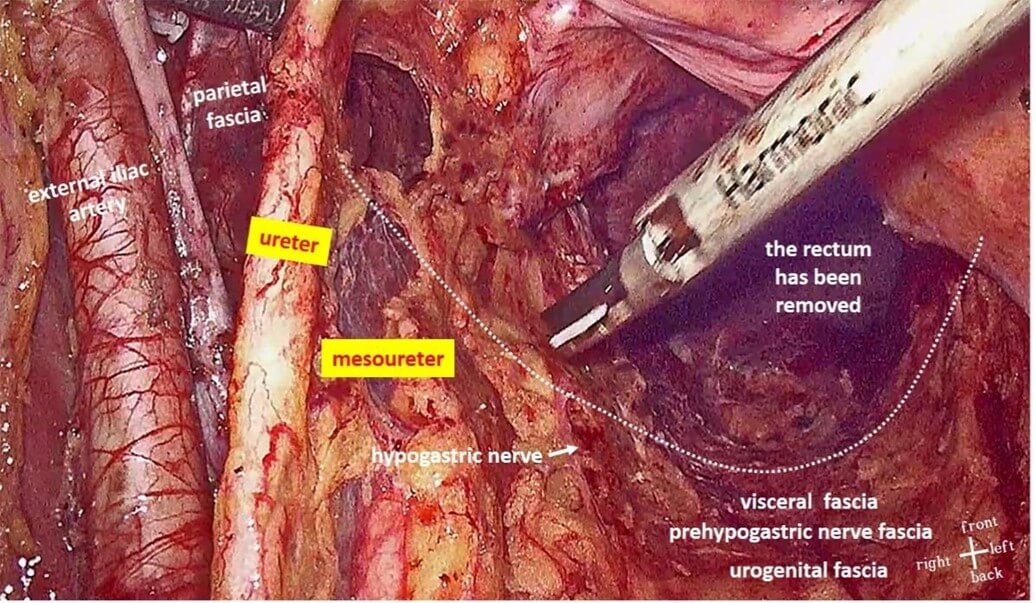
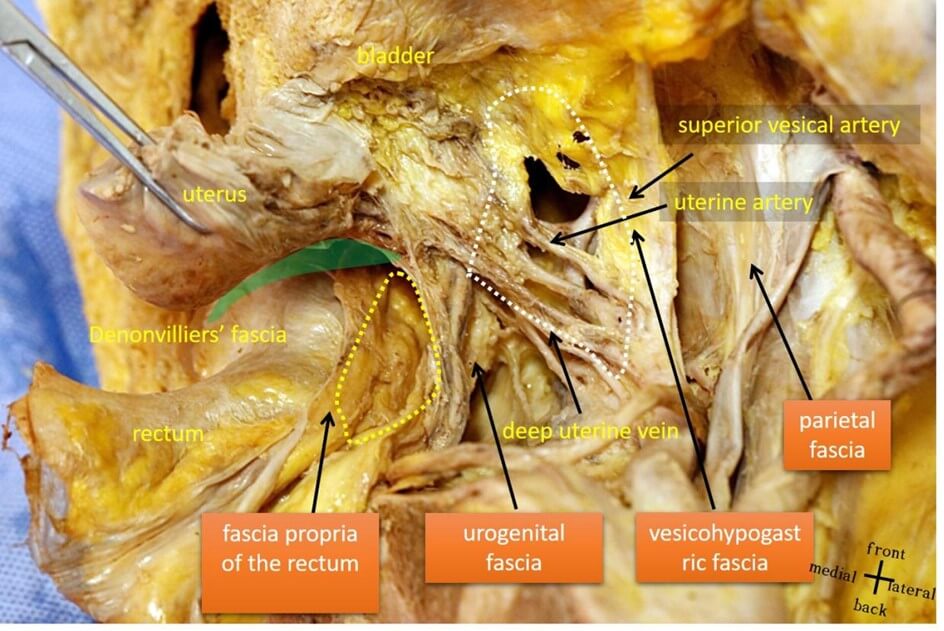
The urogenital fascia represents the continuation of the anterior and posterior renal fascia into the pelvic cavity, incorporating the ureters, gonadal vessels, hypogastric nerves, and pelvic plexus between the two layers, thus forming a "sandwich"-like structure [31, 45, 77]. It is referred to as the urinogenital fascia because this fascial layer envelopes mesodermal-origin urogenital organs, such as the kidneys and ureters, as well as reproductive organs like the testes and vas deferens. Upon extending into the pelvis, the urinogenital fascia forms a sheet encircling the rectum and stretching bilaterally to encompass the bladder, thus the two layers of the urogenital fascia are more precisely termed the visceral layer and parietal layer [76]. The visceral layer of the urinogenital fascia overlies the surface of the hypogastric nerves, and some scholars refer to it as prehypogastric nerve fascia [26, 79]. Heald posits that the hypogastric nerves reside within the visceral fascia [16, 80], while Takashi Takahashi interprets the visceral fascia as a continuous fascial layer, referred to as the visceral fascia posterior to the rectum, continuing laterally as the iliac vessel sheath, and anterior-laterally as the vesicohypogastric fascia [17]. This is consistent with the anatomical features of the urinogenital fascia, indicating that the urogenital fascia and visceral fascia represent the same anatomical structure (Figures 6, 12 & 13) [32, 61].
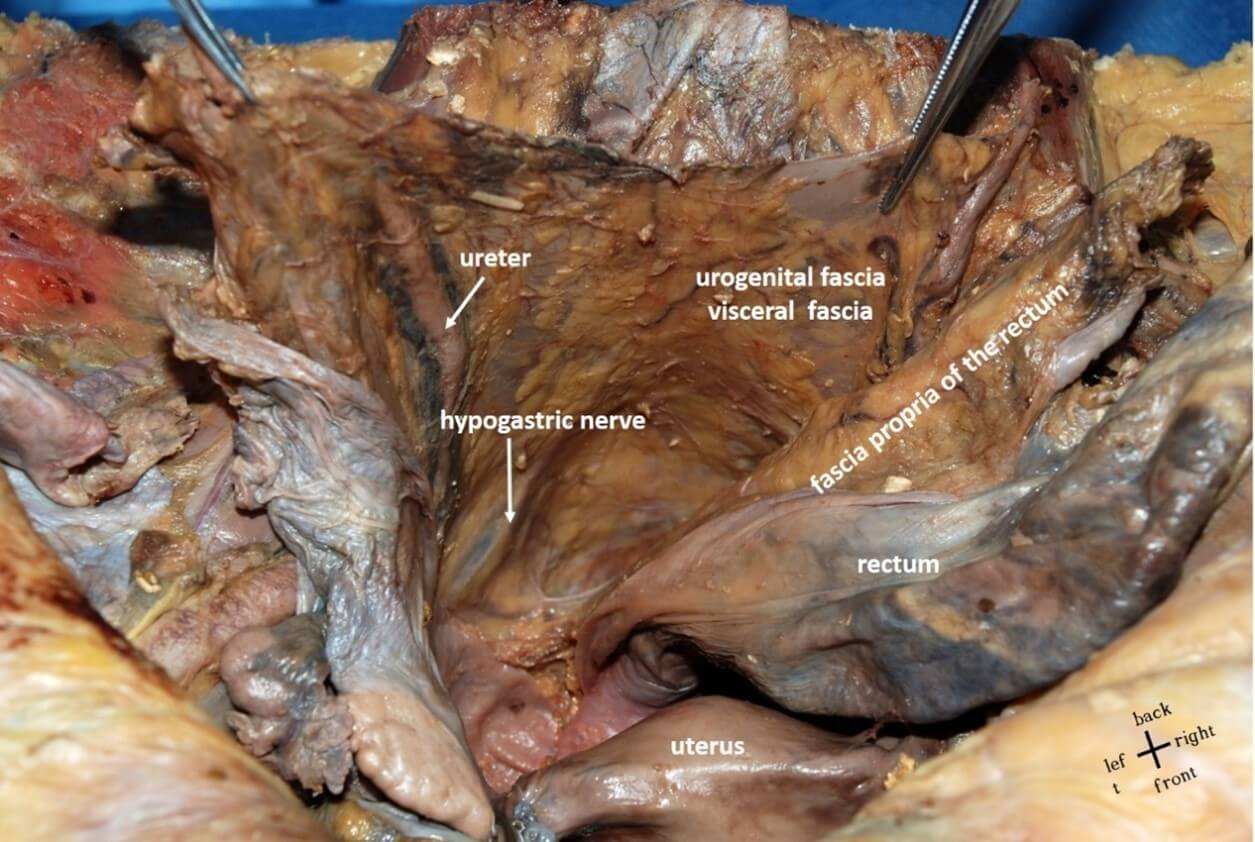
3.2.1.2.7.4. Recommendation 9
The urinogenital fascia comprises two layers, visceral and parietal, which respectively extend from the anterior and posterior renal fascia. These layers enclose the ureters, gonadal vessels, hypogastric nerves, and pelvic plexus, thereby presenting a "sandwich"-like anatomical structure.Voting approval rate: 98.6% (70/71).
3.2.1.2.8. Prehypogastric Nerve Fascia
3.2.1.2.8.1. Synonym(s)
Urogenital fascia [63, 79].
3.2.1.2.8.2. Definition
The fascia located between the rectal mesenteric fascia and presacral fascia, and positioned ventrally to the hypogastric nerves, is referred to as the prehypogastric nerve fascia [26].
3.2.1.2.8.3. Annotation
The term “prehypogastric nerve fascia” was coined by Kinugasa [26]. It is actually the visceral layer of the urogenital fascia. However, in addition to enclosing the hypogastric nerves, the two-layer structure also contain the ureters, genital vessels and pelvic plexus. Therefore, the term “prehypogastric nerve fascia” does not fully reflect its anatomical characteristics [81]. Stelzner referred to the prehypogastric nerve fascia as the inner lamella of the parietal fascia [25], which does not align with the anatomical definition of the parietal fascia (Figures 6 & 14).
3.2.1.2.8.4. Recommendation 10
The prehypogastric nerve fascia constitutes the visceral layer of theurogenital fascia. In males, it is distributed along the vas deferens and the internal surface of the seminal vesicle, reaching the seminal vesicle-prostate junction. In females, it covers the cervix and upper vagina. The prehypogastric nerve fascia connects anteriorly with Denonvilliers' fascia to form the anatomical morphology of the rectal mesentery. The pelvic plexus lies lateral to the junction between the prehypogastric nerve fascia and Denonvilliers' fascia. Voting approval rate: 97.2% (69/71).
3.2.1.2.9. Mesoureter
3.2.1.2.9.1. Synonym(s)
Uretreal leaf [82], sagittal rectal septum [83], lamina neuroducens [22], nerve root [22].
3.2.1.2.9.2. Definition
The mesoureter is a bilayered fascial structure extending dorsally and caudally from the ureters encapsulating within its layers both the ureters and the hypogastric nerves [2].
3.2.1.2.9.3. Annotation
The mesoureter, as a term in gynecological anatomy, is perceived to constitute the deep layer of the vesicouterine ligament in the anterior parametrium [47], as well as the outer layer of the posterior parametrium [55]. The ureteric fascia also demarcates the boundary between the medial and lateral pararectal spaces [84]. The ureteric fascia encompasses the hypogastric nerves [55] and comprises part of the ureter hypogastric fascia [85]. From the above description, it is apparent that the mesoureter is in fact a constituent of the urogenital fascia (Figure 15).
3.2.1.2.9.4. Recommendation 11
The mesoureter is the part of the urogenital fascia extending dorsally and caudally below the ureter. Voting approval rate: 95.8% (68/71).
3.2.1.2.10. Vesicohypogastric Fascia
3.2.1.2.10.1. Synonym(s)
Lamina ligamenti umbilicalis lateralis [83], umbilical prevesical fascia [86], umbilicoprevesical fascia [87], vesicoumbilical stalk [2].
3.2.1.2.10.2. Definition
The vesicohypogastric fascia refers to the triangular fascial structure situated between the lateral wall of the bladder, the umbilical artery, and the inferior vesical artery [17].
3.2.1.2.10.3. Annotation
The term "vesicohypogastric fascia" appears mostly in Japanese anatomy literature, often described as a bilayered structure with the visceral branches of the internal iliac artery contained between the layers [36]. However, the vesicohypogastric fascia does not cover the bladder itself but circumvents the anterolateral aspect of the bladder towards the umbilicus. Therefore, the lateral wall of the bladder does not constitute the boundary of the vesicohypogastric fascia. Additionally, the inferior boundary of the vesicohypogastric fascia terminates at the tendinous arch of pelvic fascia, rather than the inferior vesical artery [45]. The vesicohypogastric fascia overlays the external (dorsal) surface of the visceral branches of the internal iliac vessels (Figures 4 & 16) [61, 88].
3.2.1.2.10.4. Recommendation 12
The vesicohypogastric fascia is the fascial structure situated between the bladder, the umbilical artery, and the tendinous arch of the pelvic fascia. It overlays the surface of the visceral branches of the internal iliac artery, dividing the lateral lymph nodes into the external obturator lymph nodes (No. 283) and the internal iliac lymph nodes (No. 263) on the inside. Voting approval rate: 100.0%(71/71).
3.2.1.2.11. Umbilical Prevesical Fascia and Umbilical Vesical Fascia
3.2.1.2.11.1. Synonym(s)
Umbilical prevesical fascia, Charpy’s fascia [89].
3.2.1.2.11.2. Definition
The umbilical prevesical fascia is located posterior to the transversalis fascia and between the umbilicus and the inferolateral aspect of the bladder [90]. The umbilical vesical fascia extends from the vesical fascia, from the bladder to the umbilicus, encompassing within it the urachus and the umbilical artery [90].
3.2.1.2.11.3. Annotation
The umbilical prevesical fascia is a continuation of the extraperitoneal fascia or the urogenital fascia [77, 91], whereas the umbilical vesical fascia extends from the vesical fascia [70]. Both of these fasciae are located between the medial umbilical ligaments on either side. The umbilical vesical fascia is positioned posterior to the umbilical prevesical fascia, which itself is located posterior to the transversalis fascia. The umbilical vesical fascia, the umbilical prevesical fascia, and the transversalis fascia mutually fuse at the medial umbilical ligament and the umbilicus. Based on anatomical definitions, it is challenging to distinguish the anatomical boundaries of the two. This requires understanding from the perspective of Molmenti's "interfascial plane" theory, which posits that fascia itself is a separable multilayered membrane structure (Figures 4 & 17) [92].
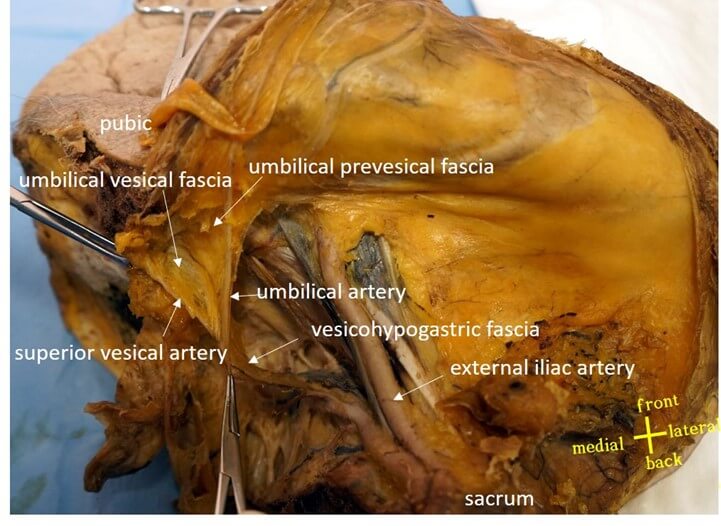
3.2.1.2.11.4. Recommendation 13
The umbilical prevesical fascia and umbilical vesical fascia represent the proximal part of the vesical hypogastric fascia. The vesical hypogastric fascia overlays the lateral aspect of the visceral branches of the internal iliac artery. Anterior and lateral to the bladder, it divides into two triangular fasciae: the deep umbilical vesical fascia and the superficial umbilical vesical anterior fascia. The umbilical vesical fascia contains the superior vesical artery covering the anterior bladder wall, while the umbilical vesical anterior fascia encapsulates the umbilical artery as it courses towards the umbilicus. Voting approval rate: 100.0%(71/71).
3.2.1.3. Fascial Sheaths and Ligaments Surrounding the Nerves and Blood Vessels of Organs
3.2.1.3.1. Lateral Ligament of the Pelvis
3.2.1.3.1.1. Synonym(s)
The neurovascular stalk [2], hypogastric sheath [6, 75], pelvic connective tissue ground bundle [83].
3.2.1.3.1.2. Definition
The connective tissue connecting the pelvic organs to the pelvic wall [22].
3.2.1.3.1.3. Annotation
The lateral ligament of the pelvis are formed by the vesical hypogastric fascia, the transverse ligament of cervix, and the lateral ligament of rectum, arranged from superior to inferior and from anterior to posterior [2]. The notion of viewing the nerves, blood vessels, and ligaments of the pelvic organs as an integrated whole has long existed in gynecological anatomy, as seen in neurovascular pedicles, connective tissue basic bundles, and hypogastric sheath [6]. In contrast, total mesorectal excision [93] and total hysterectomy [94] reflect different concepts: the ligaments or blood supply of the bladder, uterus, and rectum function as independent systems without affecting one another (Figure 18).
3.2.1.3.2. Lateral Ligament of Bladder (A04.5.03.016)
3.2.1.3.2.1. Synonym(s)
Paracystium [95].
3.2.1.3.2.2. Definition
The dense connective tissue located between the vesical neck and tendinous arch of the pelvic fascia [96].
3.2.1.3.2.3. Annotation
The anatomical term " lateral ligament of the bladder " is rarely used now. In gynecological anatomy, the portion of the anterior parametrium that extends to the bladder is the connective tissue containing the inferior vesical vessels and the distal ureter, divided into the medial vesicouterine ligament towards the head and the lateral bladder ligament towards the tail, with the ureter serving as the boundary [57, 62]. However, anatomical descriptions are inconsistent. Some consider the lateral ligament of the bladder as a thin layer of connective tissue extending caudally from the umbilical artery, dividing the paravesical space into medial and lateral compartments (Figure 4) [84].
3.2.1.3.2.4. Recommendation 14
The lateral ligament of the bladder is actually the caudal part of the vesical hypogastric fascia. Voting approval rate: 97.2% (69/71).
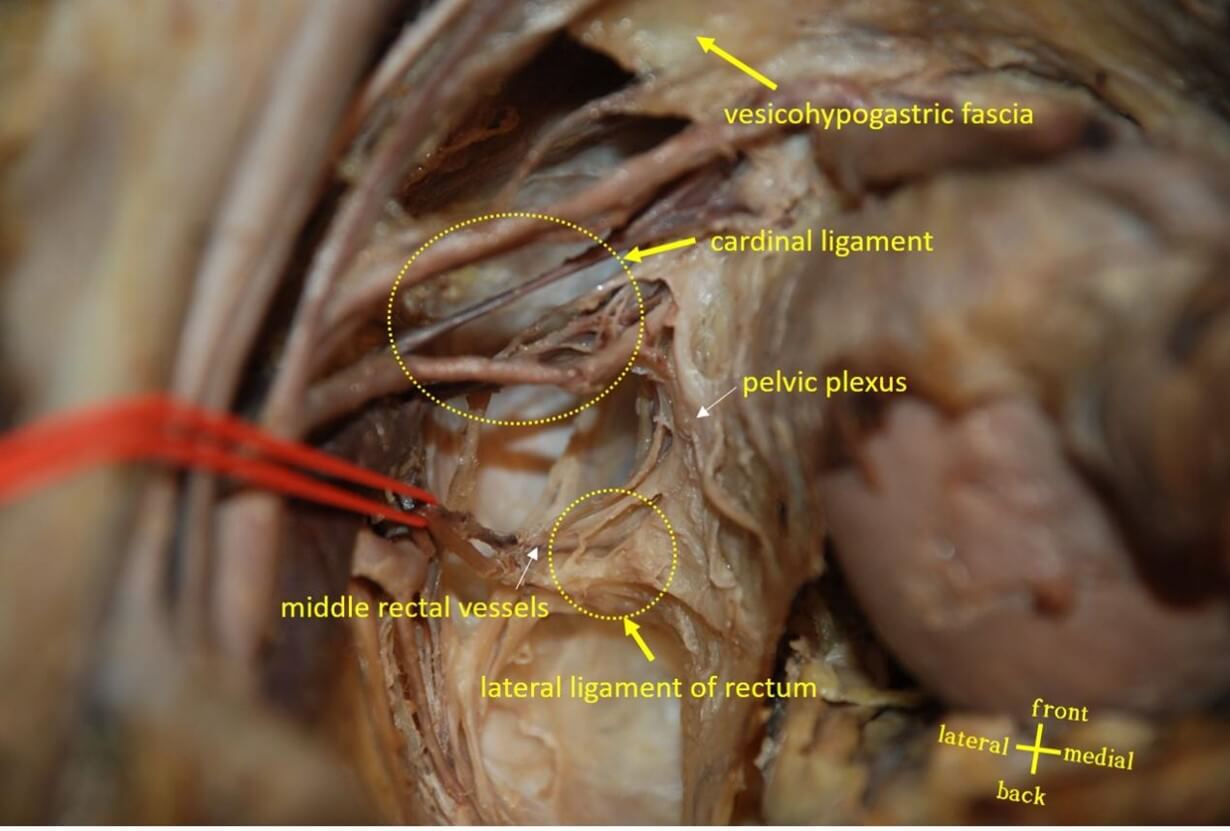
3.2.1.3.3. Lateral Ligament of Rectum (A05.7.04.016)
3.2.1.3.3.1. Synonym(s)
Rectal stalks [31], rectal pillars [10], rectal wing [97], paraproctium [31], [98], rectal pedicles [99], T-junction [27].
3.2.1.3.3.2. Definition
The fascia connecting the mesorectum to the posterolateral pelvic wall, containing the middle rectal vessels and nerves [100].
3.2.1.3.3.3. Annotation
There are two primary anatomical controversies regarding the lateral ligament of the rectum. Firstly, its position is uncertain, potentially located on the anterolateral or posterolateral side of the rectum [101]. The main reason for this controversy is the lack of recognition that the lateral ligament of rectum originates from the posterolateral pelvic sidewall adjacent to the rectum and course anteriorly and superiorly, terminating at the anterolateral proper fascia of the rectum. Secondly, its structural composition is also unclear; it may be dense connective tissue either accompanied by or lacking [66, 101, 102] neurovascular components. In recent years, it is widely considered that the lateral ligament of rectum is formed from the fusion of fasciae, such as the fusion of the proper fascia of rectum and the parietal fascia [102], the fusion of the presacral fascia and the mesorectal fascia [28], or the fusion of Denonvilliers' fascia, the rectosacral fascia, and the prehypogastric nerve fascia [63]. The second controversy arise from not comprehensively understanding the lateral ligament of rectum. Divided by the pelvic plexus, the lateral ligament of rectum actually consists of two segments: the external segment, a connective tissue containing the middle rectal vessels and nerves, and the internal segment, representing a fusion of fasciae (Figure 19) [103].
3.2.1.3.3.4. Recommendation 15
The lateral ligament of rectum is located between the posterolateral pelvic wall and the anterolateral side of the rectum. Divided by the pelvic plexus, it consists of two segments: the external segment, located between the vesical hypogastric fascia and the pelvic plexus, and the internal segment, formed by the fusion of Denonvilliers' fascia, the prehypogastric nerve fascia, and the proper fascia of rectum. Voting approval rate: 87.3%(62/71).
3.2.1.3.4. Cardinal Ligament (A09.1.03.031)
3.2.1.3.4.1. Synonym(s)
Transverse cervical ligament [47], Mackenrodt ligament [47], The web [2], Retinaculum uteri [104].
3.2.1.3.4.2. Definition
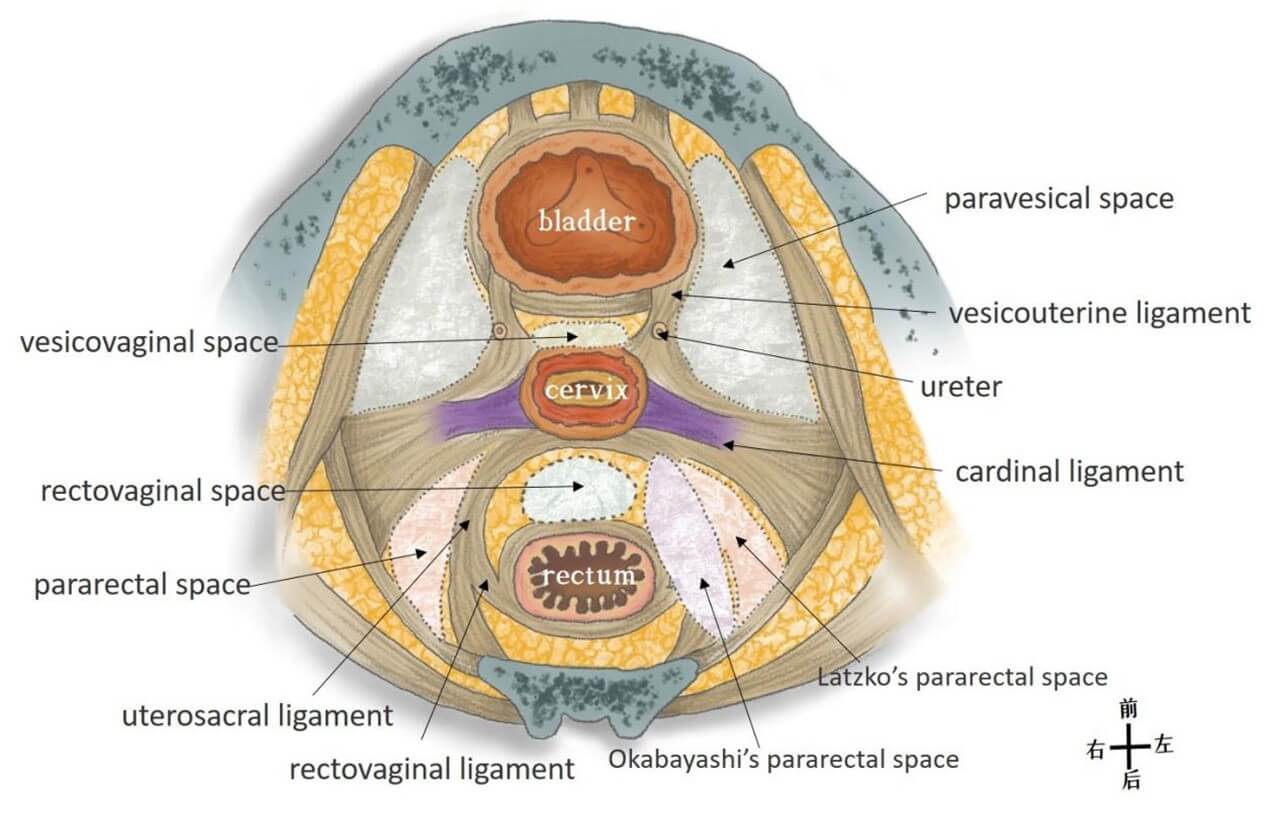
The cardinal ligament refers to the anatomical structure located between the lateral pelvic wall and the lateral side of the cervix/vagina, formed by loose connective tissue surrounding the nerves, blood vessels and lymphatic vessels [3, 6, 105].
3.2.1.3.4.3. Annotation
The anatomy of the cardinal ligament has long been contentious, with many differing terms used to describe it [106]. Japanese scholars refer to the connective tissue containing nerves and blood vessels between the paravesical and pararectal spaces as the cardinal ligament [47]. This structure encompasses, from superior to inferior, the uterine artery, deep uterine vein, middle rectal blood vessels, and pelvic splanchnic nerves [2]. Based on this understanding, Japanese scholars have proposed an important anatomical concept for preserving function in radical hysterectomy: the cardinal ligament is divided into a superficial vascular layer and a deep neural layer (which contains the pelvic splanchnic nerves) by the deep uterine vein (Figures 4, 7 & 20) [107].
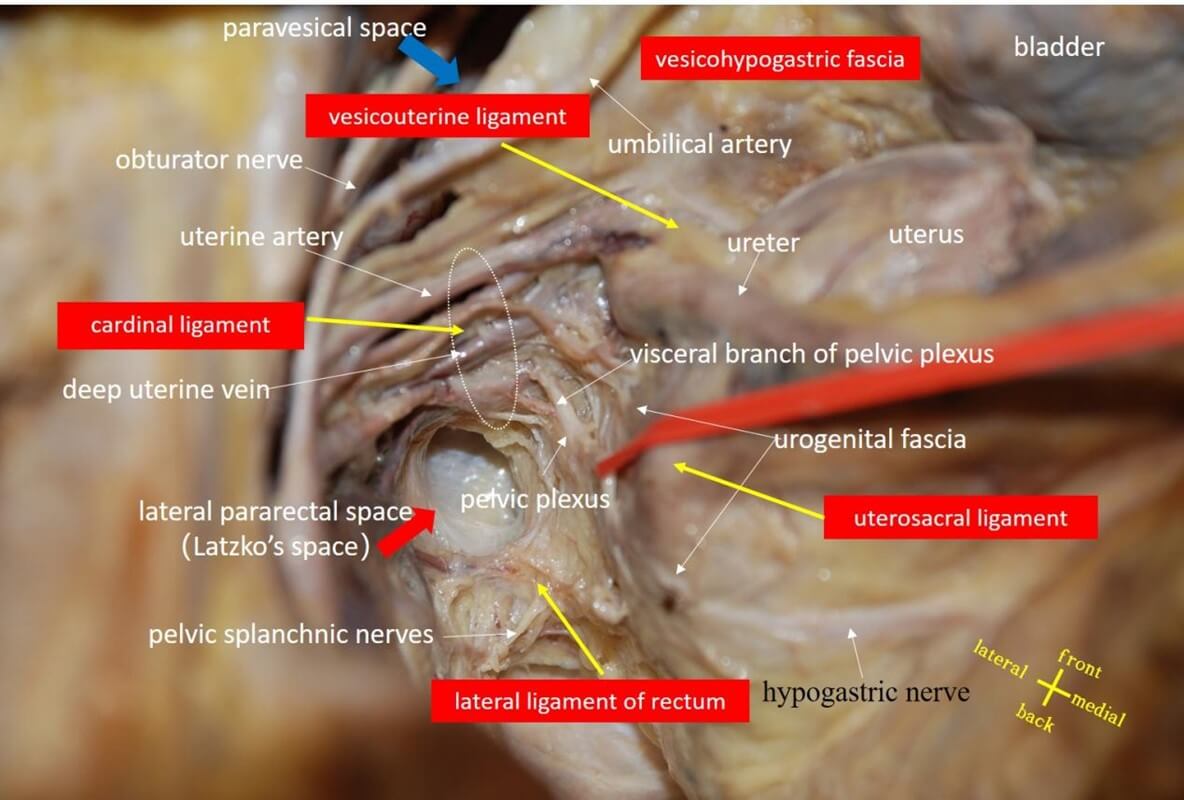
3.2.1.3.4.4. Recommendation 16
The cardinal ligament is the neural and vascular connective tissue situated laterally to the cervix/vagina, between the urogenital fascia and the vesical hypogastric fascia. Voting approval rate: 100% (71/71).
3.2.1.3.5. Parametrium (A09.1.03.021) and Paracervix (A09.1.03.022)
3.2.1.3.5.1. Synonym(s)
Parametrial web [108], cardinal ligament [109], lateral parametrium [47].
3.2.1.3.5.2. Definition
Parametrium and paracervix refer to the connective tissue containing nerves and blood vessels, extending coronally from the uterus, cervix, and lateral vagina to the lateral pelvic wall. The portion above the ureter is termed parametrium, while the part below the ureter is referred to as paracervix [22, 104, 110].
3.2.1.3.5.3. Annotation
Although parametrium and paracervix are anatomical terms published in Terminologia Anatomica [1], their definitions and usages are quite confusing. For instance, Gray's Anatomy collectively refers to parametrium and paracervix as parametrium [3], which continues downward into paracolpium. Meanwhile, the Querleu-Morrow classification uses the term paracervix to substitute for the cardinal ligament, Mackenrodt's ligament, or parametrium [57]. There are mainly three perspectives concerning the understanding of parametrium and paracervix: i) divided based on organ location, the book “Chinese Terms in Human Anatomy” defines the connective tissue at the base of the broad ligament of uterus and lateral to the cervix as the parametrium and paracervix respectively [11]; ii) demarcated by vascular landmarks, the parametrium contains the uterine artery and superficial uterine vein, while the paracervix contains the venous root, vesical inferior and vaginal vessels [22]; iii) segmented from the standpoint of ligaments, the parametrium is subdivided into anterior (vesicouterine ligament), posterior (uterosacral ligament), and lateral (cardinal ligament and paracervix) portions [111], where the lateral parametrium's cardinal ligament and paracervix are divided by the ureter (Figure 4) [62].
3.2.1.3.5.4. Recommendation 17
Parauterine tissue and paracervical tissue are located around the uterus and cervix respectively, and are neurovascular tissues between the urogenital fascia and the vesicohypogastric fascia.Voting approval rate: 98.6%(70/71).
3.2.2. Anatomical Terms Related to Parietal Fascia
3.2.2.1. Tendinous Arch of Pelvic Fascia (A04.5.03.010), Tendinous Arch of Levator Ani (A04.5.04.009)
3.2.2.1.1. Synonym(s)
Tendinous arch of pelvic fascia-arcus tendineus fasciae pelvis [112], arcus tendineus of pelvic fascia [10], conjoined arch [46], tendinous ischial arch [113], tendinous arch [114], white line [114], pelvic arcus tendinous fascia [46], tendinous arch of levator ani -arcus tendineus musculi levatoris ani [112].
3.2.2.1.2. Definition
Tendinous arch of pelvic fascia is the thickened portion of the obturator fascia located between the pubic symphysis and the sciatic spine, whose medial border is the bladder and vaginal attachment. The pelvic fascial tendon arch is an important anatomical structure for procedures involving urinary incontinence and pelvic organ prolapse [6, 20]. Tendinous arch of levator ani is located lateral to the tendinous arch of pelvic fascia, which begins 2 cm anterior to the obturator canal and converges laterally into the the tendinous arch of pelvic fascia and finally fuses with the posterior 1/3 part of the tendinous arch of pelvic fascia. Tendinous arch of levator ani is the starting point of the levator ani muscle, and is also the return point of the upper and lower fascia of the pelvic diaphragm.
3.2.2.1.3. Annotation
Many anatomical documents, including the "Human Anatomy Glossary" published in 2014, identify the tendinous arch of pelvic fascia and the tendinous arch of levator ani as the same anatomical structure [11]. In fact, they are two different anatomical structures (Figures 4, 21 & 22) [51, 22, 115].
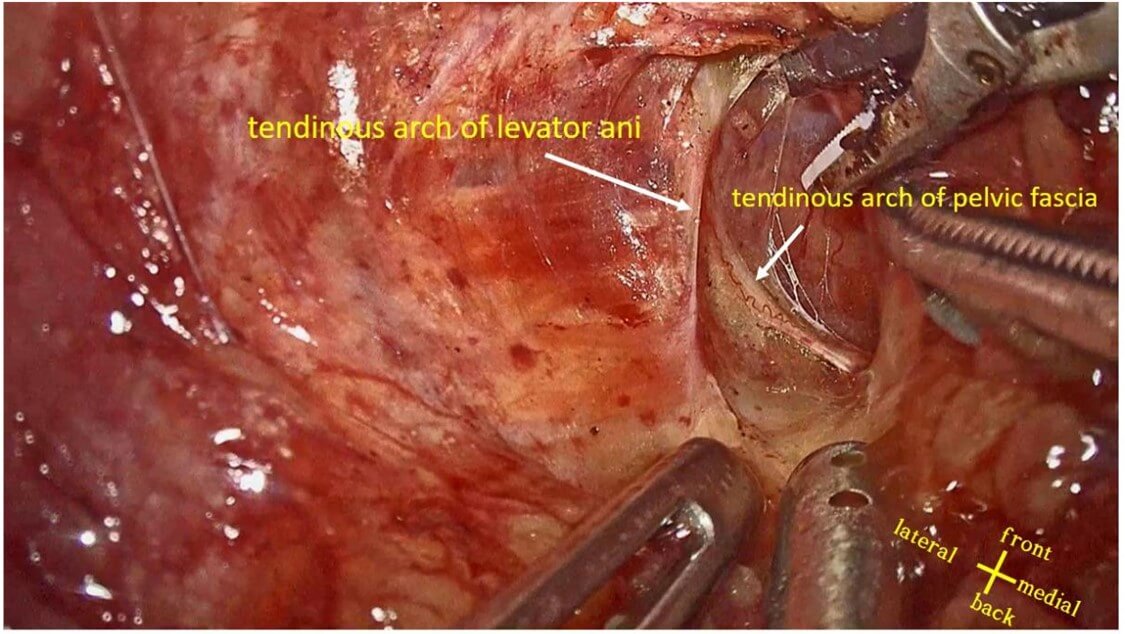
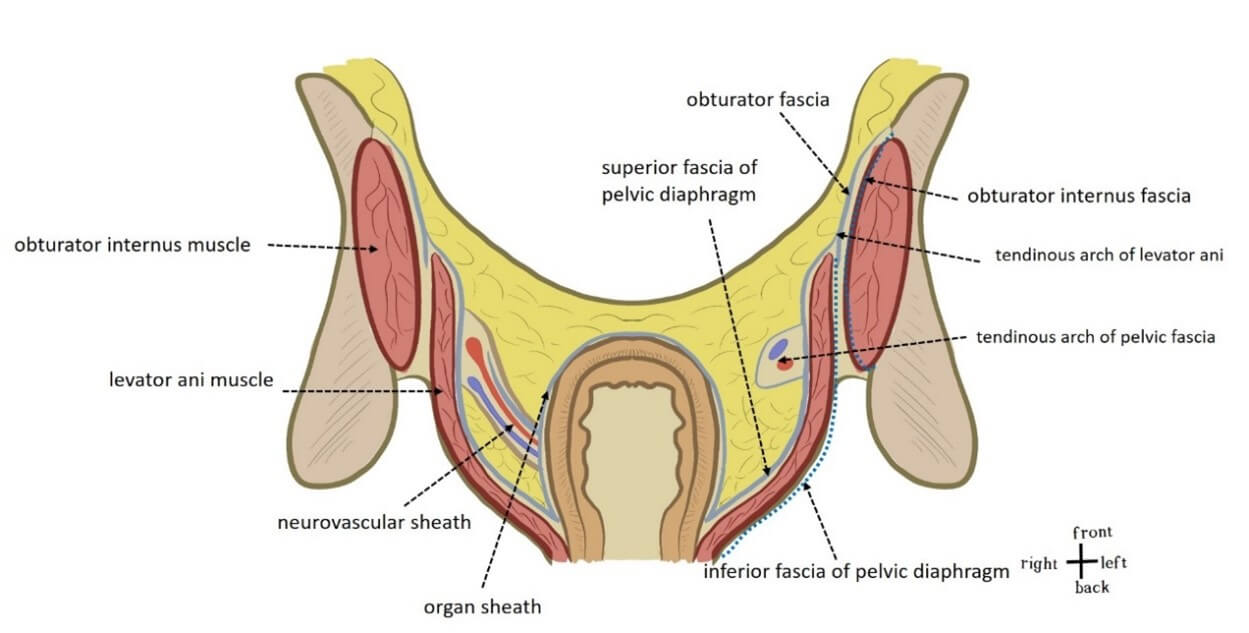
3.2.2.1.4. Recommendation 18
Although the tendinous arch of pelvic fascia and the tendinous arch of levator ani are both formed by dense and thickened pelvic parietal fascia, they are different anatomical structures. The tendinous arch of pelvic fascia is the attachment point of the vagina and bladder, while the tendinous arch of levator ani is the starting point of the levator ani muscle and the attachment point of the upper and lower fascia of the pelvic diaphragm. Voting approval rate: 100%(71/71).
3.2.2.2. Superior Fascia of Pelvic Diaphragm (A04.5.03.012)
3.2.2.2.1. Synonym
Levator fascia [46].
3.2.2.2.2. Definition
Superior fascia of pelvic diaphragm is the fascia covering the pelvic surface of the levator ani and coccygeus muscles [11].
3.2.2.2.3. Annotation
The obturator fascia is divided into three parts at the tendon arch of the levator ani muscle. One part covers the surface of the obturator internus muscle and enters the ischiorectal fossa. The other two parts cover the deep and superficial sides of the levator ani muscle and coccygeus muscle respectively to form the superior and inferior fasciae of pelvic diaphragm, respectively (Figures 4 & 22).
3.2.2.3. Presacral Fascia (A04.5.03.018)
3.2.2.3.1. Synonym
Lateral rectal fascia [6], retrorectal fascia [64],rectosacral ligament [65], Waldeyer's fascia [10].
3.2.2.3.2. Definition
Presacral fascia is refers to the thickened parietal fascia located in front of the sacrum and covering the surface of the presacral vein and median sacral artery. Presacral fascia continues laterally and caudally with the parietal fascia covering the surface of the piriformis muscle, obturator internus muscle and levator ani muscle [20, 116].
3.2.2.3.3. Annotation
The view that the presacral fascia is a multilayered structure in clinical anatomy is questionable, mainly because the existence of the urogenital fascia is not recognized. There are two representative views. One is proposed by Hollinshead and Muntean, which believes that the hypogastric nerve and pelvic plexus are included in the presacral fascia [10, 31]. In fact, the presacral fascia here should be the urogenital fascia. Another representative view was proposed by Kinugasa. The presacral fascia is divided into two layers on the side of the rectum. The superficial layer extends to the superior pelvic diaphragmatic fascia, and the deep layer merges with the prehypogastric fascia and then continues with Denonvilliers fascia in front. Therefore, the hypogastric nerve is located between the presacral fascia and the prehypogastric fascia [26]. The former view is inconsistent with the fact that the hypogastric nerve is located within the two layers of the urogenital fascia; the latter view mistakenly regards the superficial layer of the urogenital fascia as the deep layer of the presacral fascia (Figures 3 & 11) [81].
3.2.2.3.4. Recommendation 19
The presacral fascia is part of the parietal fascia and covers the surface of the presacral vein and median sacral artery. Voting approval rate: 98.6%(70/71).
3.2.3. Anatomical Terms Related to the Space
3.2.3.1. Pararectal Fossa (A10.1.02.514)
3.2.3.1.1. Synonym
Pararectal space [111].
3.2.3.1.2. Definition
Pararectal fossa is the space located between the rectum/uterus and the internal iliac vessels, bounded anteriorly by the main ligament and posteriorly by the sacrum [111].
3.2.3.1.3. Annotation
Pararectal fossa appears more often as pararectal space in anatomy literature, especially in gynecological anatomy literature. The pararectal space is bounded by the ureter and is divided into the medial pararectal space (Okabayashi space) and the lateral pararectal space (Latzko space) [111]. Gynecological surgery dissects the hypogastric nerve and the uterine artery through Okabayashi's space and Latzko's space, respectively (Figures 8 & 23) [117].

3.2.3.1.4. Recommendation 20
The medial pararectal hiatus is located between the fascia propria of the rectum and the visceral layer of the urogenital fascia; and the lateral pararectal hiatus is located between the parietal layer of the urogenital fascia and the vesicohypogastric fascia. Voting approval rate: 100%(71/71).
3.2.3.2. Paravesical Fossa (A10.1.02.502)
3.2.3.2.1. Synonym
Paraventricular space [22].
3.2.3.2.2. Definition
Paravesical fossa appears more frequently in the anatomical literature as the paravesical space. The paravesical space is bounded laterally by the parietal fascia (obturator fascia) on the surface of the obturator internus muscle and the external iliac vessels, medially by the bladder and vagina, posteriorly by the cardinal ligament, anteriorly by the pubic bone, and inferiorly by the levator ani muscle [48].
3.2.3.2.3. Annotation
The paravesical space is divided into lateral and medial parts by the umbilical artery. During surgery, the obturator lymph nodes can be dissected in the lateral space, and the uterine artery can be ligated at the root and parauterine tissue can be dissected in the medial space (Figures 8 & 23) [118].
3.2.3.2.4. Recommendation 21
The paravesical space is the space located between the vesicohypogastric fascia and pelvic parietal fascia. Voting approval rate: 100%(71/71).
3.2.3.3. Posterior Pubic Space (A10.1.01.003), Retroinguinal Space
3.2.3.3.1. Synonym
Retropubic space prevesical space [118], space of Retzius [119], retroinguinal space-iliac area [120].
3.2.3.3.2. Definition
The retropubic space is bounded anteriorly by the pubic bone, posteriorly by the bladder, and laterally by the tendinous arch of pelvic fascia [117]. The retroinguinal space is a triangular space located between the fascia iliaca, parietal peritoneum, and transversalis fascia [121].
3.2.3.3.3. Annotation
The retropubic space (Retzius space) is a potential surgical space filled with loose connective tissue and venous plexus. The Santorini venous plexus forms the floor of the Retzius space [122]. There are many different views on the membranous anatomy of the retropubic space, which can be located between the transversalis fascia and the preumbilical bladder fascia [77], or between the retrorectus abdominis sheath and the anterior umbilical bladder fascia [123], or between the deep and superficial layers of the preperitoneal fascia [124]. Some scholars also believe that the retropubic space is formed by multiple gaps composed of multiple layers of fascia [125]. The retropubic space and the retroinguinal space (Bogros space) are generally bounded by the line connecting the inferior epigastric artery and the vas deferens, while the retropubic space and the paravesical space are generally bounded by the umbilical artery (Figures 4 & 24) [117].
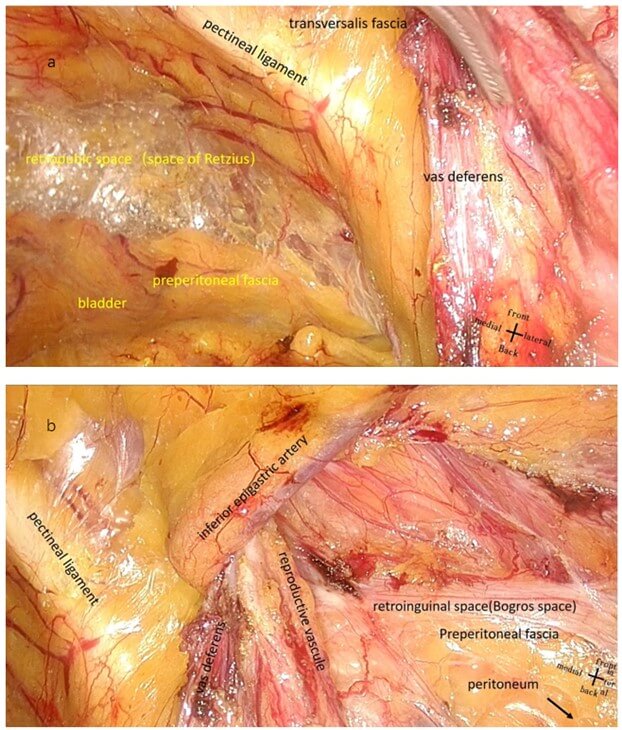
3.2.3.3.4. Recommendation 22
The retropubic space is located between the transversalis fascia and the preperitoneal fascia, while the retroinguinal space is located between the preperitoneal fascia and the peritoneum. The two spaces are not in the same plane. Voting approval rate: 100%(71/71).
3.2.3.4. Retrorectal Space and Presacral Space
3.2.3.4.1. Synonym
None.
3.2.3.4.2. Definition
The space between the rectum and sacrococcygeal bone [119].
3.2.3.4.3. Annotation
Most anatomical literature considers the retrorectal space to be the presacral space. From the perspective of membrane anatomy, the retrorectal space refers to the space between the proper rectal fascia and the presacral fascia [58, 126], and is divided into the upper and lower spaces by the rectosacral fascia [127]. However, some scholars believe that with the urogenital fascia as the boundary, this space can be divided into the retrorectal space on the ventral side and the presacral space on the dorsal side (Figures 5 & 25) [27, 128].
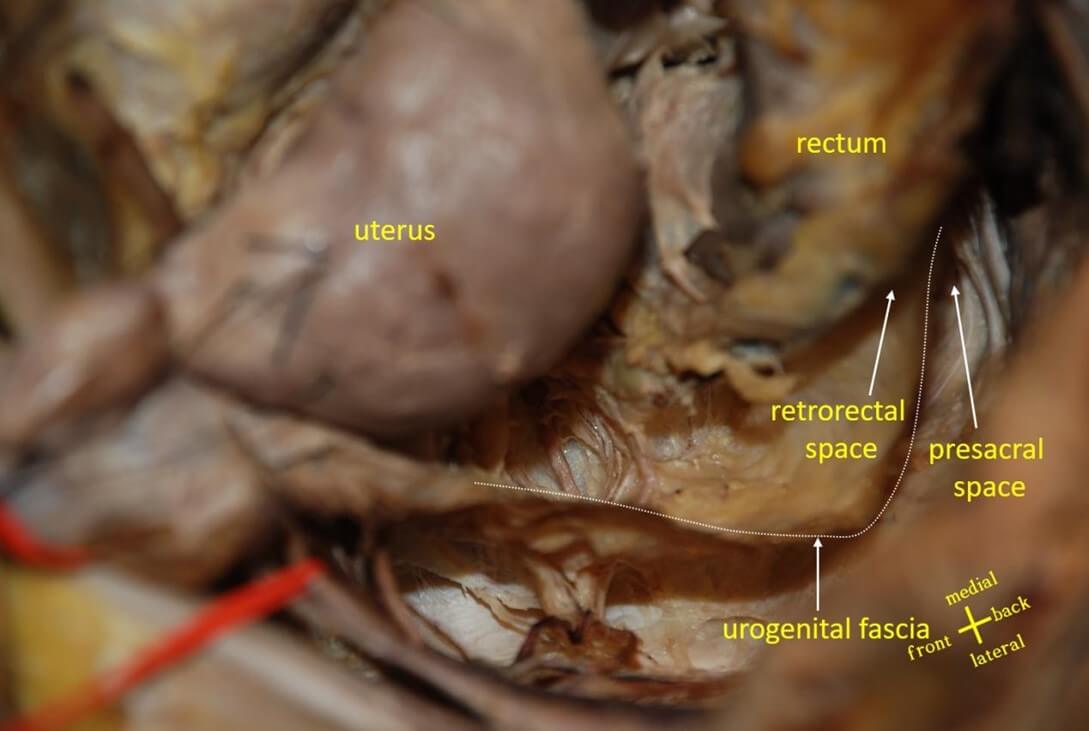
3.2.3.4.4. Recommendation 23
The retrorectal space is located between the fascia propria of the rectum and the visceral layer of the urogenital fascia, and the presacral space is located between the parietal layer of the urogenital fascia and the presacral fascia. Voting approval rate: 98.6%(70/71).
3.2.3.5. The Yabuki Fourth Space and Okabayashi Paravaginal Space
3.2.3.5.1. Synonym
None.
3.2.3.5.2. Definition
The Yabuki fourth space is located between the end of the ureter, vesical nerves, blood vessels and the medial vagina [84, 111]. The Okabayashi paravaginal space is located between the blood vessels of the vagina and cervix (paravaginal tissues) and the posterior lobe of the vesicouterine ligament [111, 129].
3.2.3.5.3. Annotation
Many anatomical literatures believe that the fourth space and the paravaginal space are the same space [49, 84], but in fact they are not the same concept [130]. Yabuki et al. [131] proposed the concept of the fourth space in 2000, which is located above and medial to the ureter, and it is possible to incise the superficial layer of the vesicouterine ligament along the fourth space to the beginning of the ureteral tunnel [132]. Okabayashi paravaginal space is the space between the cervix uterus and the ureter in order to separate the deeper layer of the vesicouterine ligament, and this space is located beneath and medial to the ureter. The posterior lobe of the vesicouterine ligament can be cut between the paravaginal space and the paravesical space (Figure 26) [132].
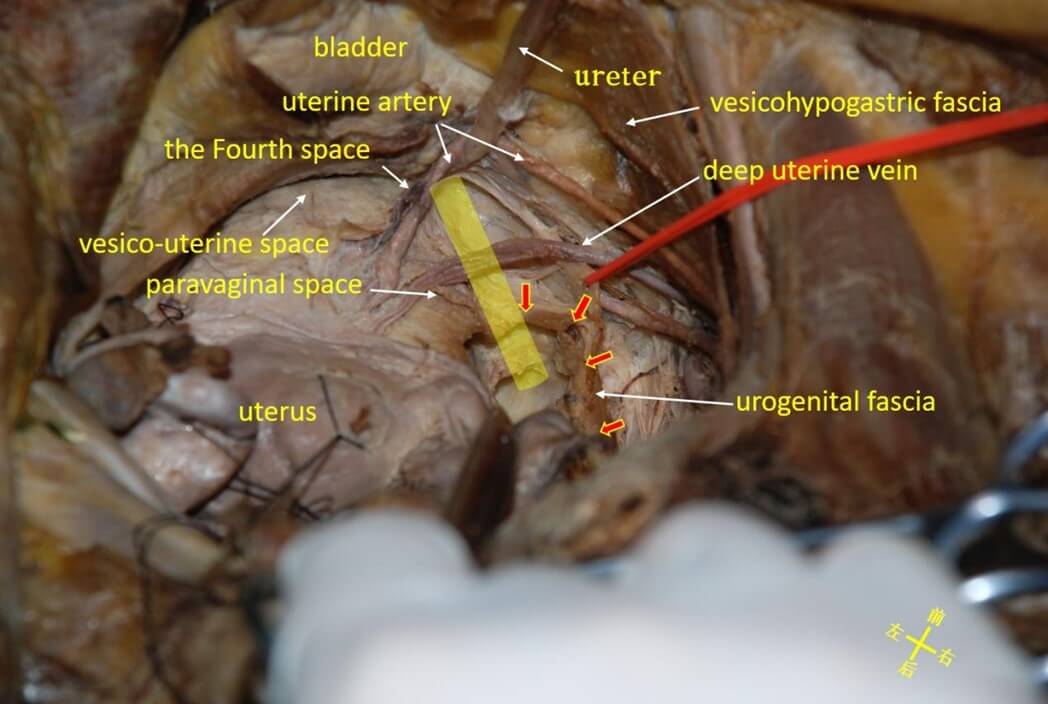
Note: the yellow column is the normal anatomical position of the ureter and the red arrow is the urogenital fascia.
3.2.3.5.4. Recommendation 24
The Yabuki fourth space and the Okabayashi paravaginal space are not the same space. The Yabuki fourth space is located above the end of the ureter, between the urogenital fascia and the hypogastric fascia. The Okabayashi paravaginal space is located beneath the end of the ureter, between the vagina and the urogenital fascia. Approval rate: 98.6% (70/71).
3.2.3.6. Obturator Space
3.2.3.6.1. Synonyms
Laterovascular space [117], lumbosacral space [133], medial psoas space [117].
3.2.3.6.2. Definition
The obturator space is located within the paravesical space. The medial boundary is the external iliac vessel, the lateral boundary is the iliac fascia and the genitofemoral nerve covering the psoas major muscle, the ventral boundary is the venae circumflexa ilium profunda, and the dorsal boundary is the furcation of the common iliac artery (Figure 27) [134].
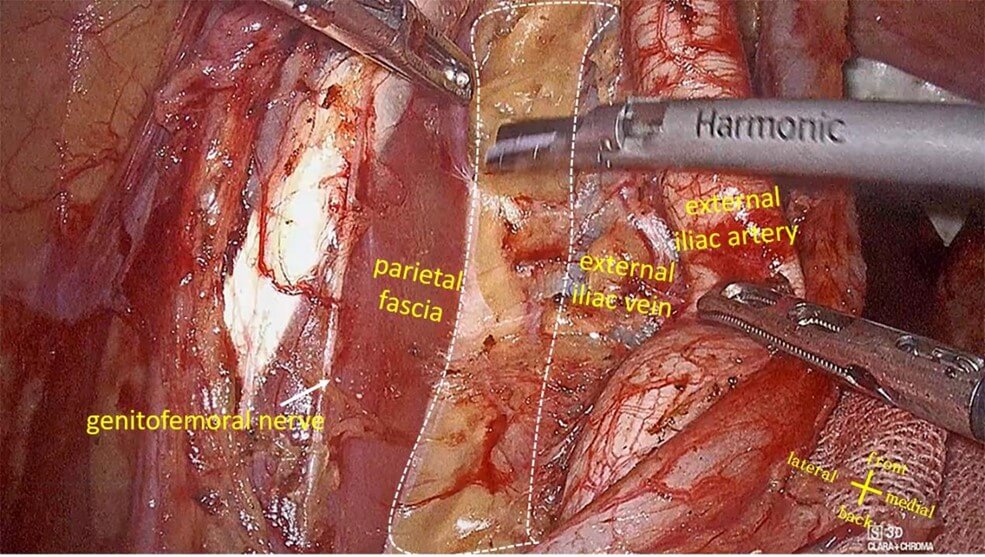
Note: the white dotted line is the obturator gap.
3.2.4. Others
3.2.4.1. Anococcygeal Body, Anococcygeal Ligament (A04.5.04.016)
3.2.4.1.1. Synonym
Hiatal ligament [135].
3.2.4.1.2. Definition
The connective tissue behind the anal canal connecting the tailbone to the anal canal [11].
3.2.4.1.3. Annotation
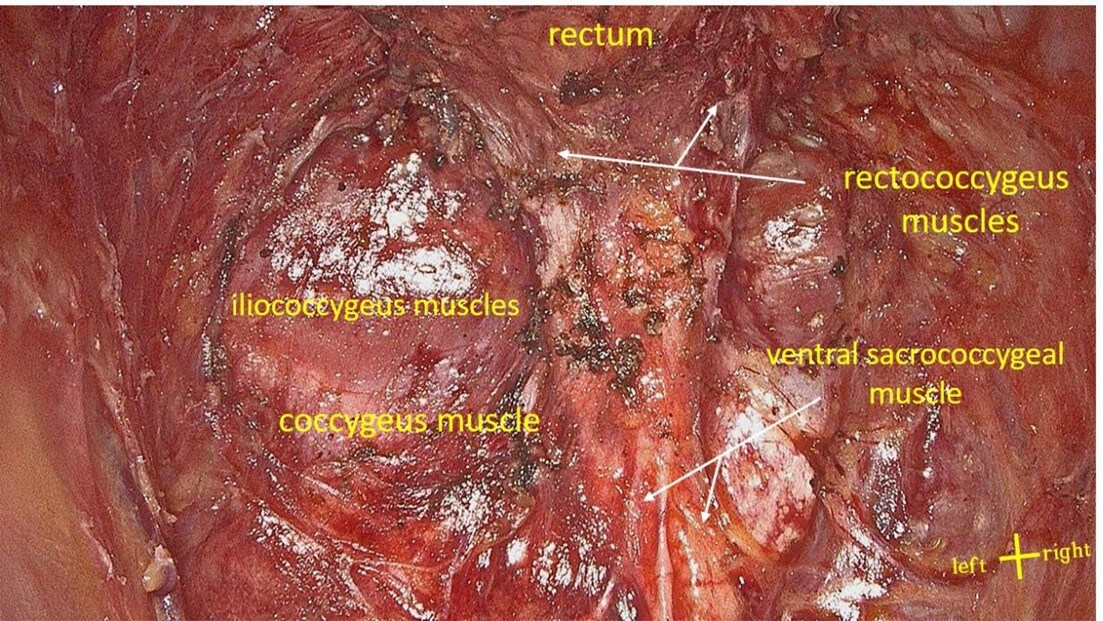
Most classical anatomical monographs believe that the anococcygeal ligament is located on the dorsal side of the musculus levator ani [4-7], but Gray's Anatomy shows different illustrations of the anococcygeal ligament. Thus, anococcygeal ligaments are depicted in different places on the ventral or dorsal side of the musculus levator ani [3]. Recent views tend to divide the procycaudal ligaments into two parts: the ventral part and the dorsal part. The ventral part is thick and loose, located between the anterior sacral fascia and the associative longitudinal muscle. The dorsal part is thin and dense, located between the tailbone and the external sphincter [136]. However, some Japanese scholars habitually call the ventral part of the anococcygeal ligament the Hiatal Ligaments [137]. The Hiatal ligament is not a real ligament, but a part of the longitudinal rectal muscle, and is that the longitudinal rectal muscle separates into fan-shaped muscle fiber bundles before passing through the levator ani hiatus and is attached and fixed to the levator ani muscle. These muscle bundles are the thickest at the 6 o'clock and 12 o'clock directions, and are actually the rectococcygeus and recto-urethralis, respectively [138]. The naming of the rectococcggeus and recto-urethralis incorporates the anatomical location and tissue composition to avoid ambiguity (Figure 28).
3.2.4.1.4. Recommendation 25
The so-called ventral anococcygeal ligament is composed of the ventral sacrococcygeal muscle and the rectococcygeus muscle. The ventral sacrococcygeal muscle extends from the sacrum to the coccyx, and the rectococcygeal muscle extends from the coccyx to the rectal wall. The generliazed Hiatal ligament includes the rectococcggeus behind the rectum and the recto-urethralis in front, both of which are composed of smooth muscle. It is recommended to abandon the names of Hiatal ligament and ventral anococcygeal ligament. Approval rate: 87.3% (62/71).
3.2.4.2. Mesometrium (A10.1.02.506)
3.2.4.2.1. Definition
The broad ligament of the uterus can be divided into the mesosalpinx above, the mesovarium behind, and the mesometrium below. The mesometrium is the largest part of the broad ligament, extending from the pelvic floor to the ovarian ligament and the body of the uterus, with the uterine artery passing between its two layers of peritoneum [139].
3.2.4.2.2. Annotation
The introduction of total mesometrial resection (TMMR) completely changed the classical concept of mesometria [140]. The mesometrium is divided into two parts, the vascular mesometrium and the ligamentous mesometrium, which extends dorsolateral and includes the blood vessels, lymphatic vessels, lymph nodes, and loose connective tissue of the uterus and vagina. The ligamentous mesometrium is a three-dimensional dense connective tissue that extends dorsally and downwardly, and appears as a horseshoe in cross section. The ligamentous mesometrium is adjacent to the mesorectum and appears as an arc covering the anterolateral side of the mesorectum and then connects with the coccyx. The muscle surface is continuous with the intrapelvic fascia on the surface of the coccygeus muscle. The ligamentous mesometrium is actually the posterior layer of the broad ligament, the rectuterine ligament, the rectovaginal ligament, and the rectovaginal septum in traditional anatomy (Figure 29) [140-142].
Note: the yellow dotted line is the ligamentous mesometrium and the white dotted line is the vascular mesometrium.
3.2.4.3. Mesorectum
3.2.4.3.1. Definition
The surrounding fat of the rectum and its blood vessels, nerves and lymph are wrapped by fascia to form an "envelope"-like anatomical structure called the mesorectum [3].
3.2.4.3.2. Annotation
Mesentery was first proposed by Maunsell et al. [143]. Although it does not meet the anatomical definition of mesorectum, nor is it included in Terminologia Anatomica. However, due to the widespread clinical use of the TME proposed by Heald, mesorectum has become a widely accepted clinical anatomical term. Classic anatomy believes that the rectovesical (vaginal) septum and the visceral fascia (pre-hypogastric nerve fascia, visceral layer of urogenital fascia) constitute the anatomical form of the mesorectum [26, 61]. In recent years, it has been found that the fascia propria of the rectum and the visceral fascia are actually two different fascia layers, thus changing the understanding of the anatomical morphology of mesorectum (Figures 16 & 30) [32].
3.2.4.3.3. Recommendation 26
The mesorectum is an "envelope-like" structure wrapped by the fascia propria of the rectum, and contains related blood vessels, lymphoid tissue, nerves, fat and other tissues. The fascia propria of the rectum continues with the colonic fascia cranially and fuses with the pelvic parietal fascia caudally. Approval rate: 94.4% (67/71).
Acknowledgements
Thanks to the following experts who participated in the writing and discussion: Gong Chen (Sun Yat-sen University Cancer Center); Jingbo Chen (Shandong Provincial Qianfoshan Hospital); Wenping Chen (Xi’an Daxing Hospital); Yuanguang Chen (The First Affiliated Hospital of Guangzhou Medical University); Zhifen Chen (Fujian Medical University Union Hospital); Zhaocheng Chi (Jilin Cancer Hospital);Dechang Diao (Guangdong Provincial Hospital of Chinese Medicine);Ruoxu Dou (The Fifth Affiliated Hospital of Sun Yat-sen University); Peng Du (Xinhua Hospital Affiliated To Shanghai Jiaotong University School of Medicine); Wei Fu (The Affiliated Hospital of Xuzhou Medical University); Junyi Han (Shanghai East Hospital of Tongji University); Ping Huang (Sir Run Run Hospital,Nanjing Medical University); Jianzheng Jie (China-Japan Friendship Hospital); Hangyu Li (The Forth Affiliated Hospital of China Medical University); Jianwen Li (Ruijin Hospital Shanghai Jiaotong University School Of Medicine); Jun Li(Guang’anmen Hospital, China Academy of Chinese Medical Sciences); Ming Li(Peking University Shougang Hospital); Shaotang Li (The First Affiliated Hospital of Wenzhou Medical University ); Xinxiang Li (Fudan University Shanghai Cancer Center); Xinyu Li (Quanzhou First Hospital); Guole Lin (Peking Union Medical College Hospital); Qian Liu (Cancer Hospital, Chinese Academy of Medical Sciences );Jihui Luo (People's Hospital of Hunan Province); Feng Sun (The First Affiliated Hospital, Guangzhou University of Traditional Chinese Medicine); Yi Sun (People's Hospital of Tianjin); Deyan Tan (Department of Anatomy, Histoembryology, School of Basic Medical Sciences, Fudan University); Erjiang Tang (Yangpu Hospital Affiliated to Tongji University); Xin Wang (Peking University First Hospital);Hao Wang (Naval Medical University, Changhai Hospital); Kai Wang (The Affiliated Hospital of Xuzhou Medical University); Liming Wang (Shenzhen Hospital, Chinese Academy of Medical Sciences Cancer Hospital); Quan Wang (First Affiliated Hospital of Jilin University); Yanan Wang (Southern Medical University Nanfang Hospital); Zheng Wang (Union Hospital, Tongji Medical College, Huazhong University of Science and Technology);Yongyou Wu (The Second Affiliated Hospital of Soochow University); Jianbin Xiang (Fudan University Huashan Hospital); Zhongshi Xie (China-Japan Union Hospital of Jilin University); Danfeng Xu: Ruijin Hospital Shanghai Jiaotong University School Of Medicine; Dong Xu (Second Affiliated Hospital, Zhejiang University School of Medicine); Yanchang Xu (Putian First Hospital); Su Yan (Qinghai University Affiliated Hospital); Dongdong Yang (Fourth Affiliated Hospital of Harbin Medical University); Liu Yang (Jiangsu Cancer Hospital); Lu Yin (Tenth People's Hospital of Tongji University); Xiangyang Yu (Tianjin Nankai Hospital); Hong Zhang (Shengjing Hospital of China Medical University ); Jianping Zhang (Second Affiliated Hospital of Nanjing Medical University); Jian Zhang (Naval Medical University, Changzheng Hospital); Ren Zhao (Ruijin Hospital, Shanghai Jiaotong University School Of Medicine); Zongheng Zheng (Sun Yat-sen University Third Affiliated Hospital); Xiaojun Zhou (The First Affiliated Hospital of Soochow University); Yuping Zhu (Zhejiang Cancer Hospital); Ping Zhu (Traditional Chinese Medicine Hospital of Jiangsu Province). The authors also thank Jiaqi Wang (Yangpu Hospital Affiliated to Tongji University) and Huihong Jiang (Yangpu Hospital Affiliated to Tongji University) for their contributions in the preparation of the article, and Chang Le (The Second People's Hospital of Changzhou City) for his contribution in drawing the anatomical drawings.
Conflicts of Interest
None.
REFERENCES
[1] Monkhouse
WS “Terminologia Anatomica. International Anatomical Terminology.” 1998.
[2] Yoshihiko
Yabuki, Hiromasa Sasaki, Noboru Hatakeyama, et al. “Discrepancies between
classic anatomy and modern gynecologic surgery on pelvic connective tissue
structure: Harmonization of those concepts by collaborative cadaver
dissection.” Am J Obstet Gynecol, vol. 193, no. 1, pp. 7-15, 2005. View
at: Publisher Site | PubMed
[3] D'Antoni,
Anthony, V. “Gray's Anatomy, the Anatomical Basis of Clinical Practice, 41st
edition. Clinical anatomy: official journal of the American Association of
Clinical Anatomists & the British Association of Clinical Anatomists.” vol.
29, no. 2, pp. 264-265, 2016.
[4] Clemente,
Carmine D “Anatomy : a regional atlas of the human body.” 6th ed.,
International ed: Anatomy : a regional atlas of the human body / 6th ed.,
international ed.
[5] Snell
“Clinical Anatomy By Regions.” 2012.
[6] D'Antoni
AV “Clinically Oriented Anatomy.” 7th Edition, by Keith L. Moore, Arthur F.
Dalley II, and Anne M. R. Agur, Baltimore, MD: Lippincott Williams &
Wilkins, 1134 pages, 2014.
[7] Anderson,
James E “Grant's Atlas of Anatomy.” Wolters Kluwer Health/Lippincott Williams
& Wilkins.
[8] Olinger
AB “Human Gross Anatomy.”
[9] Hinman
F, Stempen PH “Hinman's atlas of urosurgical anatomy: Hinman's atlas of
urosurgical anatomy.”
[10]
Hollinshead WH “Anatomy For
Surgeons.” Plastic & Reconstructive Surgery vol. 42, no. 6, 1957.
[11]
Human Anatomy and Histoembryology
Terminology Approval Committee. Human Anatomy Terminology. 2014: Human Anatomy
Terminology. 2014.
[12]
Cui Huixian, Li Ruixi. “Regional
anatomy: regional anatomy.” 2018.
[13]
R. Atkinson Stoney “The Anatomy of
the Visceral Pelvic Fascia.” J Anat Physiol, vol. 38, no. Pt 4, pp. 438-447,
1904. View at: PubMed
[14]
Michal Otcenasek, Vaclav Baca,
Ladislav Krofta, et al. “Endopelvic Fascia in Women: Shape and Relation to
Parietal Pelvic Structures.” Obstet Gynecol, vol. 111, no. 3, pp.
622-630, 2008. View at: Publisher Site | PubMed
[15]
Carla Stecco, Maria Martina Sfriso,
Andrea Porzionato, et al. “Microscopic anatomy of the visceral fasciae.” J
Anat, vol. 231, no. 1, pp. 121-128, 2017. View at: Publisher
Site | PubMed
[16]
R J Heald, B J Moran “Embryology and
anatomy of the rectum.” Semin Surg Oncol, vol. 15, no. 2, pp. 66-71,
1998. View at: Publisher Site | PubMed
[17]
Takahashi Takashi, Han Fanghai
“Radical resection of colorectal cancer: radical resection of colorectal cancer.”
2003.
[18]
M Diop 1, B Parratte, L Tatu, et al.
“"Mesorectum": the surgical value of an anatomical approach.” Surg
Radiol Anat, vol. 25, no. 3-4, pp. 290-304, 2003. View at: Publisher Site | PubMed
[19]
R Bendavid, D Howarth “Transversalis
fascia rediscovered.” Surg Clin North Am, vol. 80, no. 1, pp. 25-33,
2000. View at: Publisher Site | PubMed
[20]
H Fritsch, H Hötzinger “Tomographical
anatomy of the pelvis, visceral pelvic connective tissue, and its
compartments.” Clin Anat, vol. 8, no. 1, pp. 17-24, 1995. View at: Publisher
Site | PubMed
[21]
Mélanie Roch, Nathaly Gaudreault,
Marie-Pierre Cyr, et al. “The Female Pelvic Floor Fascia Anatomy: A Systematic
Search and Review.” Life (Basel), vol. 11, no. 9, pp. 900, 2021. View
at: Publisher
Site | PubMed
[22]
Alfredo Ercoli, Vincent Delmas,
Francesco Fanfani, et al. “Terminologia Anatomica versus unofficial
descriptions and nomenclature of the fasciae and ligaments of the female
pelvis: A dissection-based comparative study.” Am J Obstet Gynecol, vol.
193, no. 4, pp. 1565-1573, 2005. View at: Publisher Site | PubMed
[23]
Panagiotis N Skandalakis, Odyseas
Zoras, John E Skandalakis, et al. “Transversalis, endoabdominal, endothoracic
fascia: who's who?” Am Surg, vol. 72, no. 1, pp. 16, 2006. View at: PubMed
[24]
T Sato, M Hashimoto “Morphological
analysis of the fascia lamination of the trunk.” Bull Tokyo Med Dent Univ,
vol. 31, no. 1, pp. 21-32, 1984. View at: PubMed
[25]
Sigmar Stelzner, Tillmann Heinze,
Taxiarchis K Nikolouzakis, et al. “Perirectal Fascial Anatomy: New Insights
Into an Old Problem.” Dis Colon Rectum, vol. 64, no. 1, pp. 91-102,
2021. View at: Publisher Site | PubMed
[26]
Y Kinugasa, G Murakami, D Suzuki, et
al. “Histological identification of fascial structures posterolateral to the
rectum.” Br J Surg, vol. 94, no. 5, pp. 620-626, 2007. View at: Publisher
Site | PubMed
[27]
Werner Hohenberger, Michael Parker
“Lower Gastrointestinal Tract Surgery.” Vol. 2, Open procedures: Vol. 2, Open
procedures, 2021.
[28]
J García-Armengol, S García-Botello,
F Martinez-Soriano, et al. “Rewiew of the anatomic concepts in relation to the
rectrorectal space and endopelvic fascia:Waldeyer'fascia and the rectosacral
fascia.” Colorectal Dis, vol. 10, no. 3, pp. 298-302, 2008. View at: Publisher Site | PubMed
[29]
Jong Min Lee, Nam Kyu Kim “Essential
Anatomy of the Anorectum for Colorectal Surgeons Focused on the Gross Anatomy
and Histologic Findings.” Ann Coloproctol, vol. 34, no. 2, pp. 59-71,
2018. View at: Publisher
Site | PubMed
[30]
Mahmoud N Kulaylat “Mesorectal
excision: Surgical anatomy of the rectum, mesorectum, and pelvic fascia and
nerves and clinical relevance.” World Journal of Surgery, 2015;vol. 5,
no. 1, pp. 14, 2015. View at: Publisher Site
[31]
V Muntean “The surgical anatomy of
the fasciae and the fascial spaces related to the rectum.” Surg Radiol Anat,
vol 21, no. 5, pp. 319-324, 1999. View at: Publisher Site | PubMed
[32]
Hailong Liu, Yi Chang, Ajian Li, et
al. “Laparoscopic total mesorectal excision with urogenital fascia preservation
for mid-low rectal cancer: Anatomical basis and clinical effect - Experimental
research.” Int J Surg, vol. 99, pp. 106263, 2022. View at: Publisher Site | PubMed
[33]
Hui-Hong Jiang, Hai-Long Liu 1,
A-Jian Li, et al. “Laparoscopic lateral lymph node dissection in two fascial
spaces for locally advanced lower rectal cancer.” World J Gastroenterol,
vol. 27, no. 24, pp. 3654-3667, 2021. View at: Publisher Site | PubMed
[34]
A van Ophoven, S Roth “The Anatomy
and Embryological Origins of the Fascia of Denonvilliers: A Medico-Historical
Debate.” J Urol, vol. 157, no. 1, pp. 3-9, 1997. View at: Publisher Site | PubMed
[35]
I P Bissett, G L Hill “Extrafascial
excision of the rectum.” Semin Surg Oncol, vol. 18, no. 7, pp. 903-910,
2000. View at: Publisher Site | PubMed
[36]
Pradeep Chowbey, Davide Lomanto
“Techniques of Abdominal Wall Hernia Repair.” 2020.
[37]
Ji Hyun Kim, Yusuke Kinugasa, Si Eun
Hwang, et al. Denonvilliers' fascia revisited. Surg Radiol Anat, vol.
37, no. 2, pp. 187-197, 2015. View at: Publisher Site | PubMed
[38]
B Raychaudhuri, D Cahill “Pelvic
Fasciae in Urology.” Ann R Coll Surg Engl, vol. 90, no. 8, pp. 633-637, 2008.
View at: Publisher Site | PubMed
[39]
Robert P Myers, John C Cheville,
Wojciech Pawlina “Making anatomic terminology of the prostate and contiguous
structures clinically useful: Historical review and suggestions for revision in
the 21st century.” Clin Anat, vol. 23, no. 1, pp. 18-29, 2010. View at: Publisher
Site | PubMed
[40]
CPD D “Anatomie du périnée.” vol. 10,
pp. 105-107, 1836.
[41]
Moubin Lin, Weiguo Chen, Liang Huang,
et al. “The anatomic basis of total mesorectal excision.” Am J Surg,
vol. 201, no. 4, pp. 537-543, 2011. View at: Publisher Site | PubMed
[42]
JA TCB “Anatomical and surgical
restudy of Denonvilliers fascia.” Surg Gynecol & Obstet, vol. 80,
no. 4, pp. 373-388, 1945.
[43]
I P Bisset, K Y Chau, G L Hill
“Extrafascial excision of the rectum: surgical anatomy of the fascia propria.” Dis
Colon Rectum, vol. 43, no. 7, pp. 903-910, 2000. View at: Publisher
Site | PubMed
[44]
D D Albers, K K Faulkner, W N
Cheatham, et al. “Surgical anatomy of the pubovesical (puboprostatic)
ligaments.” J Urol, vol. 109, no. 3, pp. 388-392, 109. View at: Publisher Site | PubMed
[45]
Lin Moubin, Zhang Zhongtao “Abdominal
and pelvic surgery guidance based on modern fine anatomy: source and analysis
of membranous anatomy: Beijing: People's Medical Publishing House; pp. 58-116,
2019.
[46]
Peter C Jeppson, Sunil Balgobin,
Blair B Washington, et al. “Recommended Standardized Terminology of the
Anterior Female Pelvis Based on a Structured Medical Literature Review.” Am
J Obstet Gynecol, vol. 2019, no. 1, pp. 26-39, 2018. View at: Publisher Site | PubMed
[47]
Yoshihiko Yabuki “Twenty-first
Century Radical Hysterectomy Journey from descriptive to practical anatomy.” Gynecol
Oncol Rep, vol. 34, pp. 100623, 2020. View at: Publisher Site | PubMed
[48]
Shingo Fujii, Kenji Takakura, Noriomi
Matsumura, et al. “Precise anatomy of the vesico-uterine ligament for radical
hysterectomy.” Gynecol Oncol, vol. 104, no. 1, pp. 186-191, 2007. View
at: Publisher Site | PubMed
[49]
S. SKS “Drive safely through the
pelvis -Know your pelvic roads: The Vesico-Uterine Space.” Sri Lanka J
Obstet Gynaecol, vol. 41, pp. 89, 2019.
[50]
Denis Querleu, David Cibula, Nadeem R
Abu-Rustum “2017 Update on the Querleu–Morrow Classification of Radical
Hysterectomy.” Annals of Surgical Oncology, vol. 24, no. 11, pp.
3406-3412, 2017. View at: Publisher Site | PubMed
[51]
Sunil Balgobin, Peter C Jeppson,
Thomas Wheeler 2nd, et al. “Standardized terminology of apical structures in
the female pelvis based on a structured medical literature review.” Am J
Obstet Gynecol, vol. 222, no. 3, pp. 204-218, 2020. View at: Publisher Site | PubMed
[52]
Masaru Nakamura, Kyoko Tanaka,
Shigenori Hayashi, et al. “Local anatomy around terminal ureter related to the
anterior leaf of the vesicouterine ligament in radical hysterectomy.” Eur J
Obstet Gynecol Reprod Biol, vol. 235, pp. 66-70, 2019. View at: Publisher Site | PubMed
[53]
Noriaki Sakuragi, Gen Murakami,
Yosuke Konno, et al. “Nerve-sparing radical hysterectomy in the precision
surgery for cervical cancer.” J Gynecol Oncol, vol. 31, no. 3, pp. e49,
2020. View at: Publisher Site | PubMed
[54]
Y Shiki “Making Clear of the
Structure of Vesicouterine Ligament for Laparoscopic Radical Hysterectomy.” J Minim
Invasive Gynecol, vol. 22, no. 6, pp. S116, 2015. View at: Publisher Site | PubMed
[55]
D Cibula, N R Abu-Rustum, P
Benedetti-Panici, et al. “New classification system of radical hysterectomy:
Emphasis on a three-dimensional anatomic template for parametrial resection.” Gynecol
Oncol, vol. 122, no. 2, pp. 264-268, 2011. View at: Publisher Site | PubMed
[56]
Stefano Cosma, Domenico Ferraioli,
Marco Mitidieri, et al. “A simplified fascial model of pelvic anatomical
surgery: going beyond parametrium-centered surgical anatomy.” Anat Sci Int,
vol. 96, no. 1, pp. 20-29, 2021. View
at: Publisher Site | PubMed
[57]
Denis Querleu, C Paul Morrow
“Classification of radical hysterectomy.” Lancet Oncol, vol. 115, no. 2,
pp. 314-315, 2009. View at: Publisher Site | PubMed
[58]
Yabuki Yoshihiko “New extensive
hysterectomy.” 2014.
[59]
Angel Martín Jiménez, Anna Torrent
Colomer “An Update of Anatomical References in Total Laparoscopic Radical
Hysterectomy: From Surgical Anatomy to Anatomical Surgery.” J Minim Invasive
Gynecol, vol. 15, no. 1, pp. 4-10, 2008. View at: Publisher Site | PubMed
[60]
Hitoshi Niikura, Atsuko Katahira,
Hiroki Utsunomiya, et al. “Surgical Anatomy of Intrapelvic Fasciae and
Vesico-Uterine Ligament in Nerve-Sparing Radical Hysterectomy with Fresh
Cadaver Dissections.” Tohoku J Exp Med, vol. 212, no. 4, pp. 403-413,
2007. View at: Publisher
Site | PubMed
[61]
Liu Hailong, Lin Moubin “Key points
in understanding pelvic fascia.” Chinese Journal of Surgery, vol. 58,
no. 7, pp. 6, 2020.
[62]
Marcello Ceccaroni, Roberto Clarizia,
Giovanni Roviglione, et al. “Neuro-anatomy of the posterior parametrium and
surgical considerations for a nerve-sparing approach in radical pelvic
surgery.” Surg Endosc, vol. 27, no. 11, pp. 4386-4394, 2013. View at: Publisher Site | PubMed
[63]
Waleed M Ghareeb, Xiaojie Wang, Pan
Chi, et al. “Anatomy of the perirectal fascia at the level of rectosacral
fascia revisited.” Gastroenterology Report, vol. 10, no. 1, pp. goac001,
2022. View at: Publisher Site | PubMed
[64]
Klaas Havenga, Irene Grossmann, Marco
DeRuiter, et al. “Definition of total mesorectal excision, including the
perineal phase: technical considerations.” Dig Dis, vol. 25, no. 1, pp.
44-50, 2007. View at: Publisher
Site | PubMed
[65]
K Sato, T Sato “The vascular and
neuronal composition of the lateral ligament of the rectum and the rectosacral
fascia.” Surg Radiol Anat, vol. 13, no. 1, pp. 17-22, 1991. View at: Publisher
Site | PubMed
[66]
Nicolas Clausen, Tanja Wolloscheck,
Moritz A Konerding “How to optimize autonomic nerve preservation in total
mesorectal excision: clinical topography and morphology of pelvic nerves and
fasciae.” World J Surg, vol. 32, no. 8, pp. 1768-1775, 2008. View at: Publisher Site | PubMed
[67]
J M Church, P J Raudkivi, G L Hill
“The surgical anatomy of the rectum--a review with particular relevance to the
hazards of rectal mobilisation.” Int J Colorectal Dis, vol. 2, no. 3,
pp. 158-166, 1987. View at: Publisher Site | PubMed
[68]
Tak Lit Derek Fung, Yuichiro Tsukada
2, Masaaki Ito “Essential anatomy for total mesorectal excision and lateral
lymph node dissection, in both trans-abdominal and trans-anal perspective.” Surgeon,
vol. 19, no. 6, pp. e462-e474, 2021. View at: Publisher Site | PubMed
[69]
J García-Armengol, S García-Botello,
F Martinez-Soriano, et al. “Review of the anatomic concepts in relation to the
retrorectal space and endopelvic fascia: Waldeyer's fascia and the rectosacral
fascia.” Colorectal Disease, vol. 10, no. 3, pp. 298-302, 2008. View at:
Publisher Site | PubMed
[70]
W E Enker “Potency, Cure, and Local
Control in the Operative Treatment of Rectal Cancer.” Archives of Surgery,
vol. 127, no. 12, pp. 1396, 1992. View at: Publisher Site | PubMed
[71]
Akio Matsubara, Gen Murakami, Hitoshi
Niikura, et al. “Development of the human retroperitoneal fasciae.” Cells
Tissues Organs, vol. 190, no. 5, pp. 286-296, 2009. View at: Publisher
Site | PubMed
[72]
J F Redman “Anatomy of the
retroperitoneal connective tissue.” J Urol, vol. 130, no. 1, pp. 45-50,
1983. View at: Publisher Site | PubMed
[73]
T. S. “A morphological consideration
of the visceral fasciae with special reference to the renal fascia and its di
erentiation in the pelvic cavity.” The 14th Japanese Research Society of
Clinical Anatomy Meeting, vol. 11, pp. 82-83, 2010.
[74]
X F Yang, G H Luo, Z H Ding, et al.
“The urogenital-hypogastric sheath: an anatomical observation on the
relationship between the inferomedial extension of renal fascia and the
hypogastric nerves.” Int J Colorectal Dis, vol. 29, no. 11, pp.
1417-1426, 2014. View at: Publisher Site | PubMed
[75]
Uhlenhuth E, Day EC, et al. The
visceral endopelvic fascia and the hypogastric sheath. Surg Gynecol Obstet,
vol. 86, no. 1, pp. 9-28, 1948.
[76]
Qiu Jian, Su Junlong, Yan Likun, et
al. “Study on the level anatomy of the male urogenital layer and its clinical
significance.” Chinese Journal of Practical Surgery, vol. 41, no. 1, pp.
107-13, 2021.
[77]
Diarra B, Stoppa R, Verhaeghe P, et
al.” About prolongations of the urogenital fascia into the pelvis: An anatomic
study and general remarks on the interparietal-peritoneal fasciae.” Hernia,
vol. 1, no. 4, pp. 191-196, 1997.
[78]
Yoshihiko Yabuki “Two lateral
parametria in radical hysterectomy: History and outcome.” J Obstet Gynaecol
Res, vol. 49, no. 4, pp. 1069-1078, 2023. View at: Publisher
Site | PubMed
[79]
K. KYS “Topology of the fascial
structures inrectal surgery: Complete cancer resection and the importance of
avoiding autonomic nerve injury.” Semin Colon Rectal Surgery, vol. 21,
no. 2, pp. 95-101, 2010.
[80]
T Takahashi, M Ueno, K Azekura, et
al. “Lateral node dissection and total mesorectal excision for rectal cancer.” Dis
Colon Rectum, vol. 43, no. 10 Suppl, pp. S59-S68, 2000. View at: Publisher
Site | PubMed
[81]
Chang Yi, Liu Hailong, Lin Moubin
“Modeled operation of "two-space" lateral lymph node dissection for
rectal cancer based on membrane anatomy.” Chinese Journal of
Gastrointestinal Surgery, vol. 25, no. 4, pp. 315-320, 2022.
[82]
G Reiffenstuhl “The clinical
significance of the connective tissue planes and spaces.” Clin Obstet
Gynecol, vol. 25, no. 4, pp. 811-820, 1982. View at: Publisher Site | PubMed
[83]
Peham H, Amreich IA, Ferguson LK
“Operative gynecology.” Philadelphia: Lippincott Philadelphia; 1934.
[84]
Denis Querleu, Nicolò Bizzarri,
Francesco Fanfani, et al. “Simplified anatomical nomenclature of lateral female
pelvic spaces.” Int J Gynecol Cancer, vol. 5, pp. ijgc-2022-003531,
2022. View at: Publisher Site | PubMed
[85]
Yoshihiko Yabuki “Clinical anatomy of
the subserous layer: An amalgamation of gross and clinical anatomy.” Clin
Anat, vol. 29, no. 4, pp. 508-515, 2016. View at: Publisher
Site | PubMed
[86]
Naohito Beppu, Masataka Ikeda, Kei
Kimura, et al. “Extended Total Mesorectal Excision Based on the Avascular
Planes of the Retroperitoneum for Locally Advanced Rectal Cancer with Lateral
Pelvic Sidewall Invasion.” Dis Colon Rectum, vol. 63, no. 10, pp.
1475-1481, 2020. View at: Publisher Site | PubMed
[87]
W H ROBERTS, J HABENICHT, G
KRISHINGNER “The Pelvic and Perineal Fasciae and Their Neural and Vascular
Relationships.” Anat Rec, vol. 149, pp. 707-720, 1964. View at: Publisher
Site | PubMed
[88]
Naohito Beppu, Song Jihyung, Yuuya
Takenaka, et al. “Laparoscopic lateral pelvic lymph node dissection combined
with removal of the internal iliac vessels in rectal cancer: how to standardize
this surgical procedure.” Tech Coloproctol, vol. 25, no. 5, pp. 579-587,
2021. View at: Publisher Site | PubMed
[89]
Ceccaroni M, Roviglione G, Mautone D,
et al. “Anatomical Landmarks in Deep Endometriosis Surgery.” pp. 45-59, 2018.
[90]
Petros Mirilas, John E Skandalakis
“Surgical anatomy of the retroperitoneal spaces part II: the architecture of
the retroperitoneal space.” Am Surg, vol. 76, no. 1, pp. 33-42, 2010.
View at: PubMed
[91]
P Mirilas, A Mentessidou “The
secondary external inguinal ring and associated fascial planes: surgical
anatomy, embryology, applications.” Hernia, vol. 17, no. 3, pp 379-389,
2013. View at: Publisher Site | PubMed
[92]
E P Molmenti, D M Balfe, R Y
Kanterman, et al. “Anatomy of the retroperitoneum: observations of the
distribution of pathologic fluid collections.” Radiology, vol. 200, no.
1, pp. 95-103, 1996. View at: Publisher Site | PubMed
[93]
R J Heald, E M Husband, R D Ryall
“The mesorectum in rectal cancer surgery--the clue to pelvic recurrence?” Br
J Surg, vol. 69, no. 10, pp. 613-616, 1982. View at: Publisher Site | PubMed
[94]
M Höckel, L-C Horn, B Hentschel, et
al. “Total mesometrial resection: high resolution nerve-sparing radical
hysterectomy based on developmentally defined surgical anatomy.” Int J
Gynecol Cancer, vol. 13, no. 6, pp. 791-803, 2003. View at: Publisher Site | PubMed
[95]
Puntambekar S, Nanda S, Parikh K
“Laparoscopic Pelvic Anatomy in Females: Applied Surgical Principles.” 2019.
[96]
Marco Oderda, Romain Diamand, Simone
Albisinni, et al. “Indications for and complications of pelvic lymph node
dissection in prostate cancer: accuracy of available nomograms for the
prediction of lymph node invasion.” BJU Int, vol. 127, no. 3, pp.
318-325, 2021. View at: Publisher
Site | PubMed
[97]
Marcello Ceccaroni, Roberto Clarizia,
Francesco Bruni,, et al. “Nerve-sparing laparoscopic eradication of deep
endometriosis with segmental rectal and parametrial resection: the Negrar
method. A single-center, prospective, clinical trial.” Surg Endosc, vol.
26, no. 7, pp. 2029-2045, 2012. View at: Publisher Site | PubMed
[98]
K Richter, H Frick “Anatomy of the
visceral fascia of the pelvis from the didactic viewpoint.” Geburtshilfe
Frauenheilkd, vol. 45, no. 5, pp. 282-287, 1985. View at: Publisher Site | PubMed
[99]
Guo-Jun Wang 1, Chun-Fang Gao, Dong
Wei, et al. “Anatomy of the lateral ligaments of the rectum: a controversial
point of view.” World J Gastroenterol, vol. 16, no. 43, pp. 5411-5415,
2010. View at: Publisher Site | PubMed
[100] T
Takahashi 1, M Ueno, K Azekura, et al. “Lateral ligament: its anatomy and
clinical importance.” Semin Surg Oncol, vol. 19, no. 4, pp. 386-395,
2000. View at: Publisher Site |
PubMed
[101] O
M Jones, N Smeulders, O Wiseman, et al. “Lateral ligaments of the rectum: an
anatomical study.” Br J Surg, vol. 86, no. 4, pp. 487-489, 1999. View
at: Publisher Site | PubMed
[102] M
Nano, H M Dal Corso, G Lanfranco, et al. “Contribution to the surgical anatomy
of the ligaments of the rectum.” Dis Colon Rectum, vol. 43, no. 11, pp.
1592-1597, 2000. View at: Publisher Site | PubMed
[103] Masayuki
Ishii, Atsushi Shimizu, Alan Kawarai Lefor, et al. “Reappraisal of the lateral
rectal ligament: an anatomical study of total mesorectal excision with
autonomic nerve preservation.” Int J Colorectal Dis, vol. 33, no. 6, pp.
763-769, 2018. View at: Publisher Site | PubMed
[104] Ramanah
R, Parratte B, Arbez-Gindre F, et al. “The uterosacral complex: ligament or
neurovascular pathway? Anatomical and histological study of fetuses and
adults.” Int Urogynecol J Pelvic Floor Dysfunct, vol. 19, no. 11, pp.
1565-1570, 2008.
[105] Seif
Eid, Joe Iwanaga, Rod J Oskouian, et al. “Comprehensive Review of the Cardinal
Ligament.” Cureus, vol. 10, no. 6, pp. e2846, 2018. View at: Publisher
Site | PubMed
[106] Rajeev
Ramanah, Mitchell B Berger, Bernard M Parratte, et al. “Anatomy and histology
of apical support: a literature review concerning cardinal and uterosacral ligaments.”
Int Urogynecol J, vol. 23, no. 11, pp. 1483-1494, 2012. View at: Publisher Site | PubMed
[107] S
Sakamoto, K Takizawa “An improved radical hysterectomy with fewer urological
complications and with no loss of therapeutic results for invasive cervical
cancer.” Baillieres Clin Obstet Gynaecol, vol. 2, no. 4, pp. 953-962,
1988. View at: Publisher Site | PubMed
[108] D.
Paladini, F. Raspagliesi, R. Fontanelli, et al. “Radical surgery after
induction chemotherapy in locally advanced cervical cancer. A feasibility
study.” Int J Gynecol Cancer, vol. 5, no. 4, pp. 296-300, 1995. View at:
Publisher Site | PubMed
[109] George
Iancu, Stergios K Doumouchtsis “A historical perspective and evolution of our
knowledge on the cardinal ligament.” Neurourol Urodyn, vol. 33, no. 4,
pp. 380-386, 2014. View at: Publisher Site | PubMed
[110] Marco
Scioscia, Arnaldo Scardapane, Bruna A Virgilio, et al. “Ultrasound of the
Uterosacral Ligament, Parametrium, and Paracervix: Disagreement in Terminology
between Imaging Anatomy and Modern Gynecologic Surgery.” J Clin Med,
vol. 10, no. 3, pp. 437, 2021. View at: Publisher Site | PubMed
[111] Fujii
S, Sekiyama K “Precise Neurovascular Anatomy for Radical Hysterectomy.” 2020.
[112] B
Occelli, F Narducci, J Hautefeuille, et al. “Anatomic study of arcus tendineus
fasciae pelvis.” Eur J Obstet Gynecol Reprod Biol, vol. 97, no. 2, pp.
213-219, 2001. View at: Publisher Site | PubMed
[113] B
Mauroy, E Goullet, X Stefaniak, et al. “Tendinous arch of the pelvic fascia:
application to the technique of paravaginal colposuspension.” Surg Radiol
Anat, vol. 22, no. 2, pp. 73-79, 2000. View at: Publisher Site | PubMed
[114] D
E Derry “On the Real Nature of the so-called "Pelvic Fascia."” J
Anat Physiol, vol. 42, no. Pt 1, pp. 97-106, 1907. View at: PubMed
[115] H
Fritsch, M Zwierzina, P Riss “Accuracy of concepts in female pelvic floor
anatomy: facts and myths!” World J Urol, vol. 30, no. 4, pp. 429-435,
2012. View at: Publisher Site | PubMed
[116] al
SSHTHNe “The ASCRS textbook of colon and rectal surgery Heidelberg: Springer
Cham.” pp. 3-27, 2022.
[117] Stoyan
Kostov, Stanislav Slavchev, Deyan Dzhenkov, et al. “Avascular Spaces of the
Female Pelvis-Clinical Applications in Obstetrics and Gynecology.” J Clin
Med, vol. 9, no. 5, pp. 1460, 2020. View at: Publisher Site | PubMed
[118] De
Marchi D, Mantica G, Tafuri A, et al. “Robotic surgery in urology: a review
from the beginning to the single-site.” AME Medical Journal, vol. 7,
2021.
[119] İlker Selçuk, Burak Ersak, İlkan Tatar, et al. “Basic
clinical retroperitoneal anatomy for pelvic surgeons.” Turk J Obstet Gynecol,
vol. 15, no. 4, pp. 259-269, 2018. View at: Publisher Site | PubMed
[120] Soler
M “The minimal open preperitoneal (MOPP) approach to treat the groin hernias,
with the history of the preperitoneal approach.” Annals of Laparoscopic and
Endoscopic Surgery, vol. 2, no. 8, 2017.
[121] C
Avisse, J F Delattre, J B Flament “The inguinofemoral area from a laparoscopic
standpoint. History, anatomy, and surgical applications.” Surg Clin North Am,
vol. 80, no. 1, pp. 35-48, 2000. View at: Publisher Site | PubMed
[122] Wesevich
V, Webster EM, Baxley SE “Overcoming challenges in minimally invasive
gynecologic surgery.” Gynecology and Pelvic Medicine, vol. 3, 2020.
[123] Arregui
ME “Surgical anatomy of the preperitoneal fasciae and posterior transversalis
fasciae in the inguinal region.” Hernia, vol. 1, no. 2, pp. 101-110,
1997.
[124] Stoppa
R, Diarra B, Verhaeghe P, et al. “Some problems encountered at re-operation
following repair of groin hernias with pre-peritoneal prostheses.” Hernia,
vol. 2, pp. 35-38, 1998.
[125] Ansari
MM “Retzius Space: Not A Single Anatomical Entity: New Insights, Simplified
& Illustrated in A Laparoscopic Study during TEPP Hernioplasty for Inguinal
Hernia.” Annals of International Medical and Dental Research (AIMDR),
vol. 4, pp. 63-73, 2017.
[126] Kristina
G Hobson, Vafa Ghaemmaghami, John P Roe, et al. “Tumors of the retrorectal space.”
Dis Colon Rectum, vol. 48, no. 10, pp. 1964-1974, 2005. View at: Publisher Site | PubMed
[127] Τaxiarchis Κonstantinos Νikolouzakis, Theodoros
Mariolis-Sapsakos, Chariklia Triantopoulou, et al. “Detailed and applied anatomy for improved rectal
cancer treatment.” Ann Gastroenterol, vol. 32, no. 5, pp. 431-440, 2019.
View at: Publisher Site | PubMed
[128] Ce
Zhang, Zi-Hai Ding, Guo-Xin Li, et al. “Perirectal fascia and spaces: annular
distribution pattern around the mesorectum.” Dis Colon Rectum, vol. 53,
no. 9, pp. 1315-1322, 2010. View at: Publisher Site | PubMed
[129] Kentaro
Sekiyama, Yukiko Ando, Atsuko Taga, et al. “Laparoscopic technique for
step-by-step nerve-sparing Okabayashi radical hysterectomy.” Int J Gynecol
Cancer, vol. 30, no. 2, pp. 276-277, 2020. View at: Publisher Site | PubMed
[130] Mustafa
Zelal Muallem, Yasser Diab, Jalid Sehouli, et al. “Nerve-sparing radical
hysterectomy: steps to standardize surgical technique.” Int J Gynecol Cancer,
vol. 29, no. 7, pp. 1203-1208, 2019. View at: Publisher Site | PubMed
[131] Y
Yabuki, A Asamoto, T Hoshiba, et al. “Radical hysterectomy: An anatomic
evaluation of parametrial dissection.” Gynecol Oncol, vol. 77, no. 1,
pp. 155-163, 2000. View at: Publisher Site | PubMed
[132] Xiaoming
Yang, Jing Wang, Yiwei Wang, et al. “Surgical Technique Based on Space Anatomy
for Laparoscopic Radical Trachelectomy with Uterine Artery Preservation.” J
Laparoendosc Adv Surg Tech A, vol. 31, no. 6, pp. 705-709, 2021. View at: Publisher
Site | PubMed
[133] Marcello
Ceccaroni, Roberto Clarizia, Carlo Alboni, et al. “Laparoscopic nerve-sparing
transperitoneal approach for endometriosis infiltrating the pelvic wall and
somatic nerves: anatomical considerations and surgical technique.” Surg Radiol
Anat, vol. 32, no. 6, pp. 601-604, 2010. View at: Publisher Site | PubMed
[134] Matthew
D Barber “Contemporary views on female pelvic anatomy.” Cleve Clin J Med,
vol. 72 Suppl 4, pp. S3-S11, 2005. View at: Publisher Site | PubMed
[135] Guglielmo
Niccolò Piozzi, Hyunmi Park, Ji-Seon Kim, et al. “Anatomic Landmarks for
Transabdominal Robotic-Assisted Intersphincteric Dissection for Ultralow
Anterior Resection.” Dis Colon Rectum, vol. 64, no. 5, pp. e87-e88,
2021. View at: Publisher Site | PubMed
[136] R
Schiessel, J Karner-Hanusch, F Herbst, et al. “Intersphincteric resection for
low rectal tumours.” Br J Surg, vol. 81, no. 9, pp. 1376-1378, 1994.
View at: Publisher Site | PubMed
[137] Watanabe
Masahiko. Essentials and techniques of rectal and anal surgery. In: Zhang Hong,
editor.: Beijing: People's Medical Publishing House; 2012.
[138] Cong
Jinchun, Zhang Hong “Clinical significance and application of anatomical
research on Hiatal ligament.” Chinese Journal of Practical Surgery, vol.
39, no. 7, pp. 746-750, 2019.
[139] Hollinshead
HW “Anatomy for surgeons.” Volume 2, The thorax, abdomen and pelvis. New York:
Hoeber Harper New York; 1956.
[140] Michael
Höckel, Lars-Christian Horn, Helga Fritsch “Association between the mesenchymal
compartment of uterovaginal organogenesis and local tumour spread in stage
IB-IIB cervical carcinoma: a prospective study.” Lancet Oncol, vol. 6,
no. 10, pp. 751-756, 2005. View at: Publisher Site | PubMed
[141] M
Höckel, L-C Horn, B Hentschel, et al. “Total mesometrial resection: high
resolution nerve-sparing radical hysterectomy based on developmentally defined
surgical anatomy.” Int J Gynecol Cancer, vol. 13, no. 6, pp. 791-803,
2003. View at: Publisher Site | PubMed
[142] Attibele Palaksha Manjunath, Shivarudraiah Girija “Embryologically based resection of cervical cancers: a new concept of surgical radicality.” J Obstet Gynaecol India, vol. 62, no. 1, pp. 5-14, 2012. View at: Publisher Site | PubMed
[143] M L Corman “Sphincter-Saving Operations.” Surg Clin North Am, vol. 53, no. 2, pp. 405-415, 1973. View at: Publisher Site | PubMed